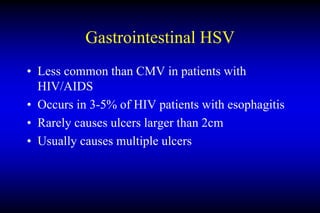
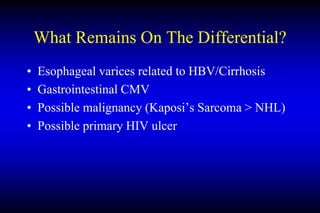
This document discusses the differential diagnosis and risk factors for an upper gastrointestinal bleed in an HIV-positive patient. Key points include: (1) CMV, HSV, primary HIV ulcers, Kaposi's sarcoma, and lymphoma are more likely causes of ulcers or masses in the GI tract of an HIV+ patient; (2) The patient's CD4 count, esophageal ulcer, varices, gastric polyp, and bluish GEJ lesion suggest diagnoses of gastrointestinal CMV, esophageal varices related to cirrhosis, or Kaposi's sarcoma are most probable; (3) Co-infections like CMV are more common in HIV patients with low CD4 counts and can cause severe