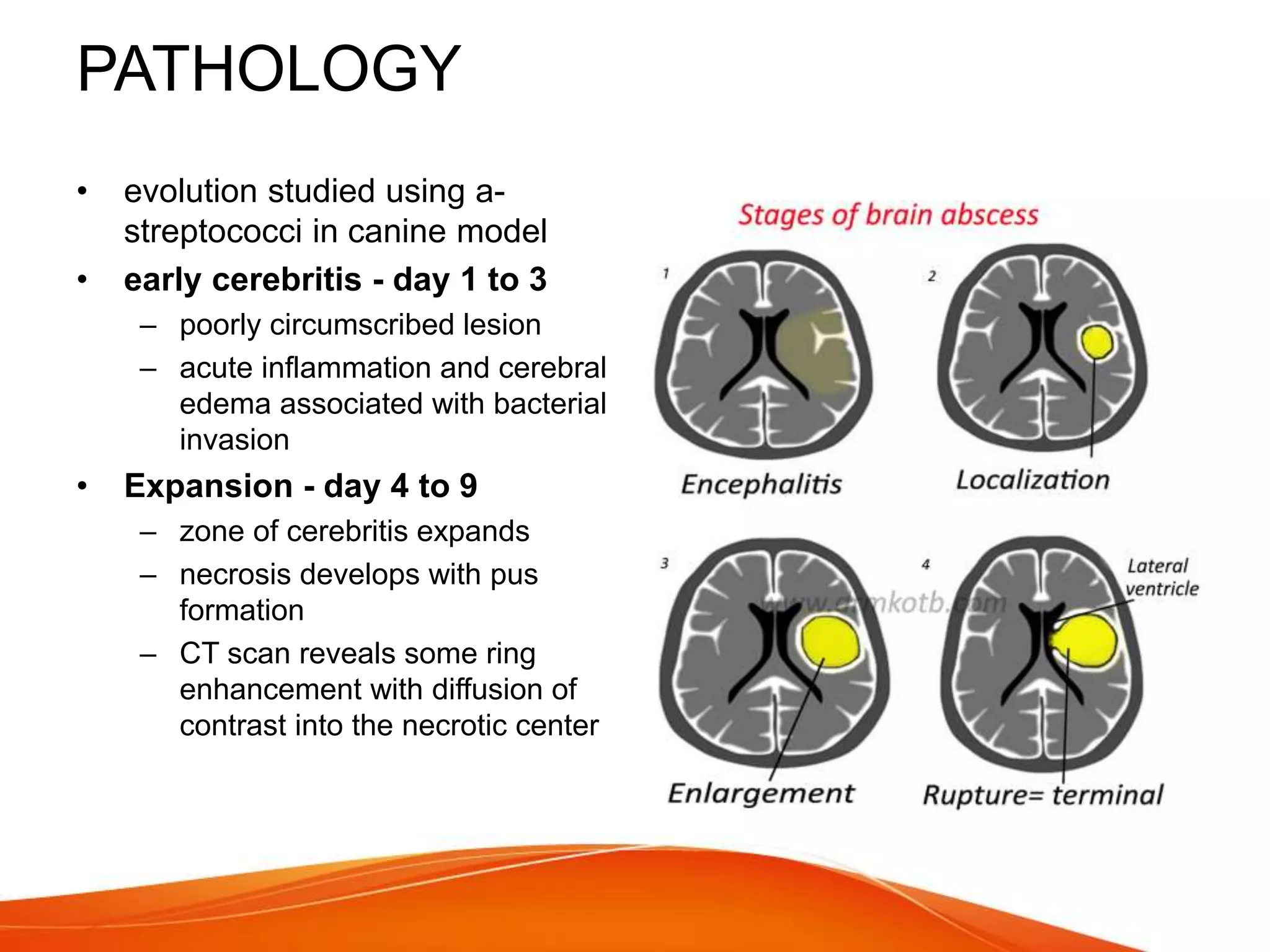
This document summarizes key information about pyogenic brain abscesses:
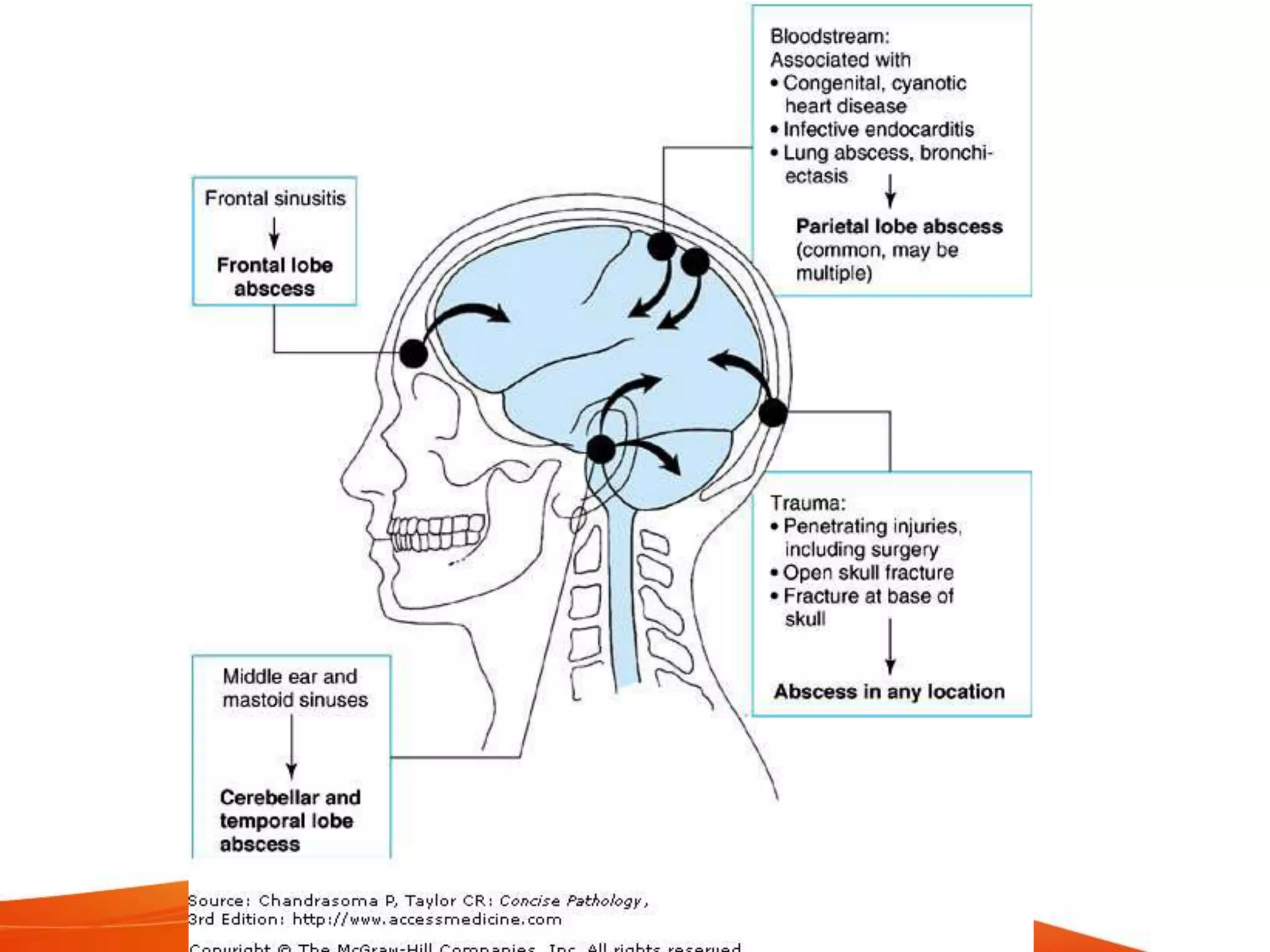
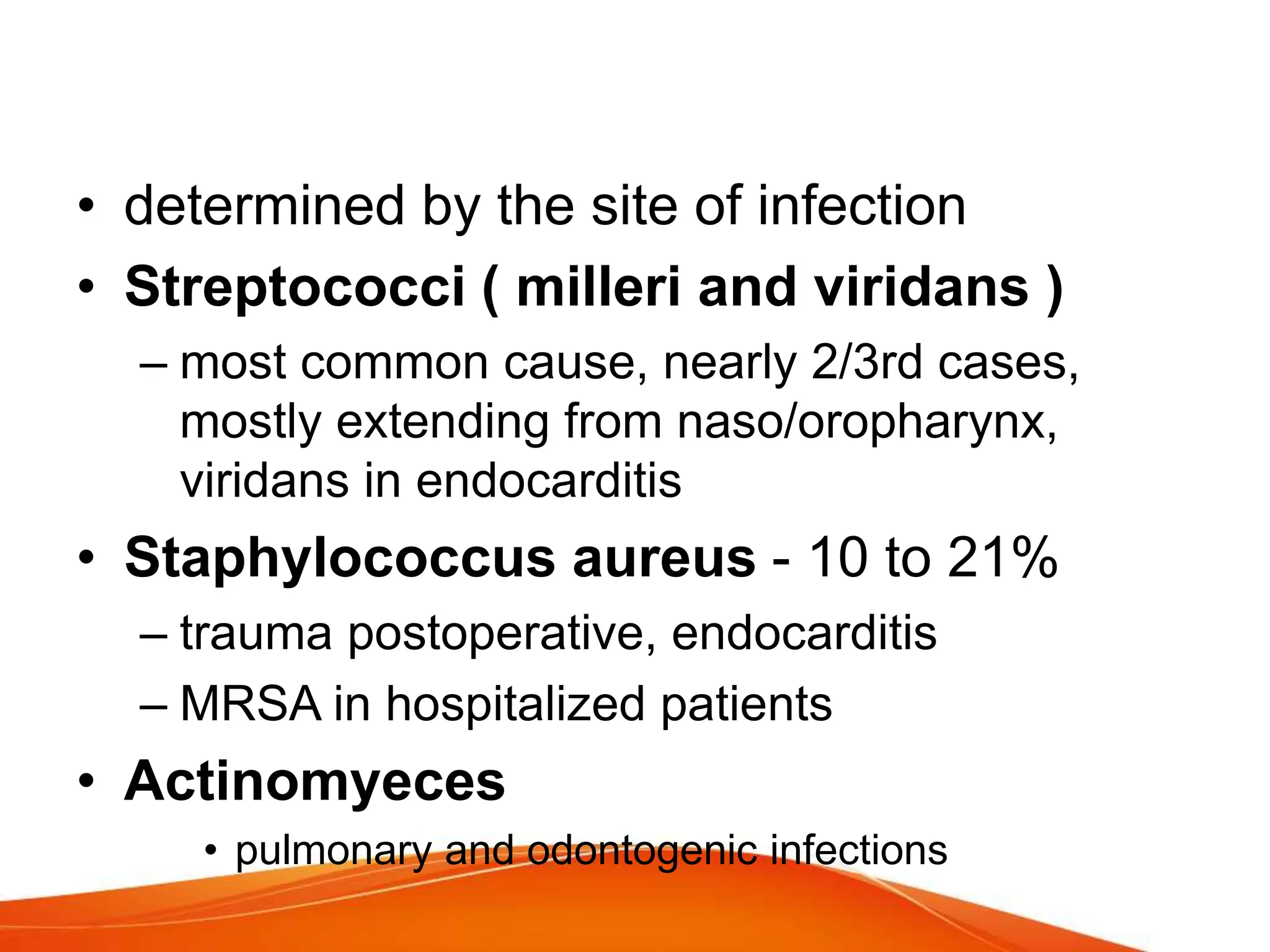
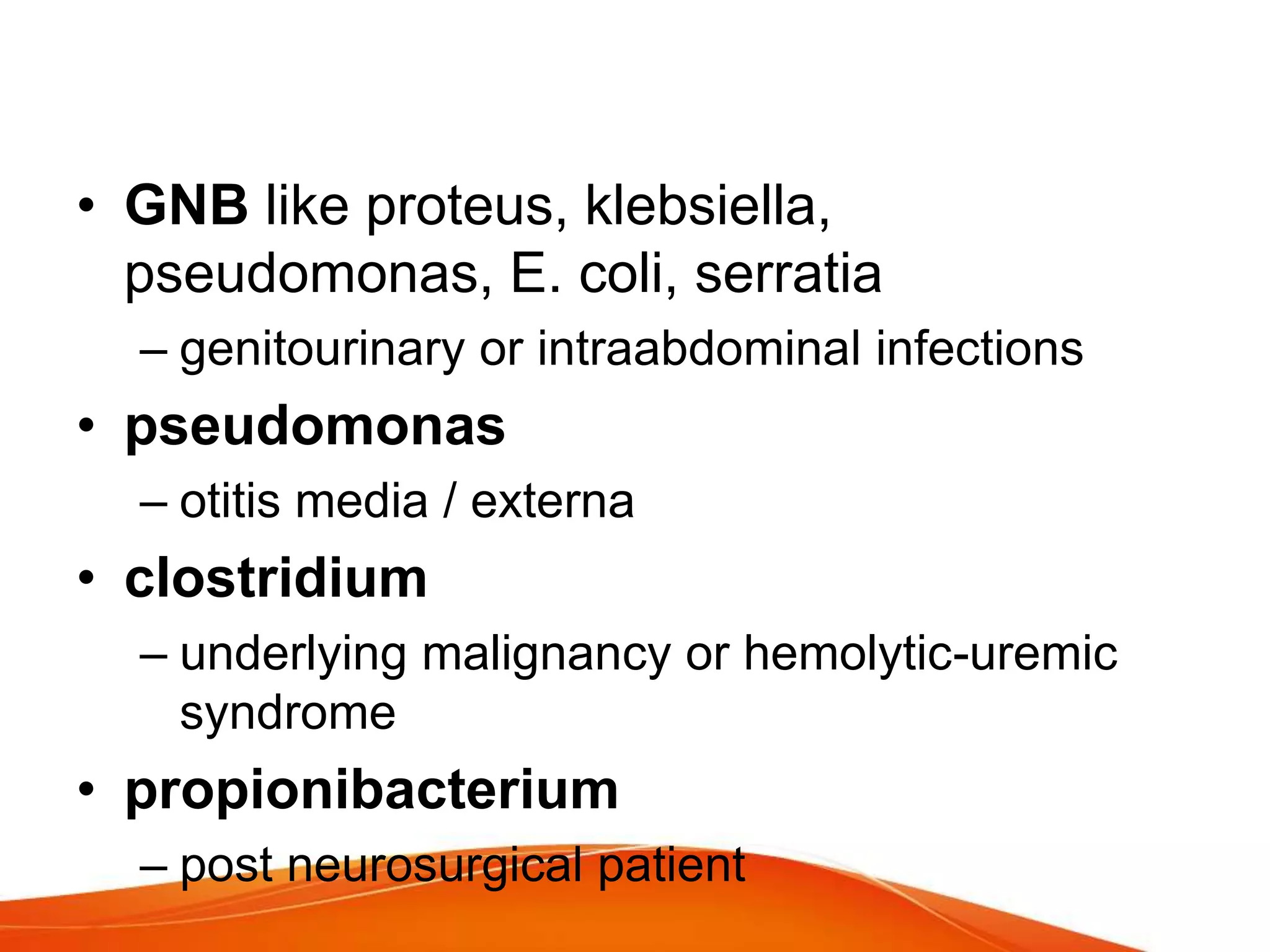
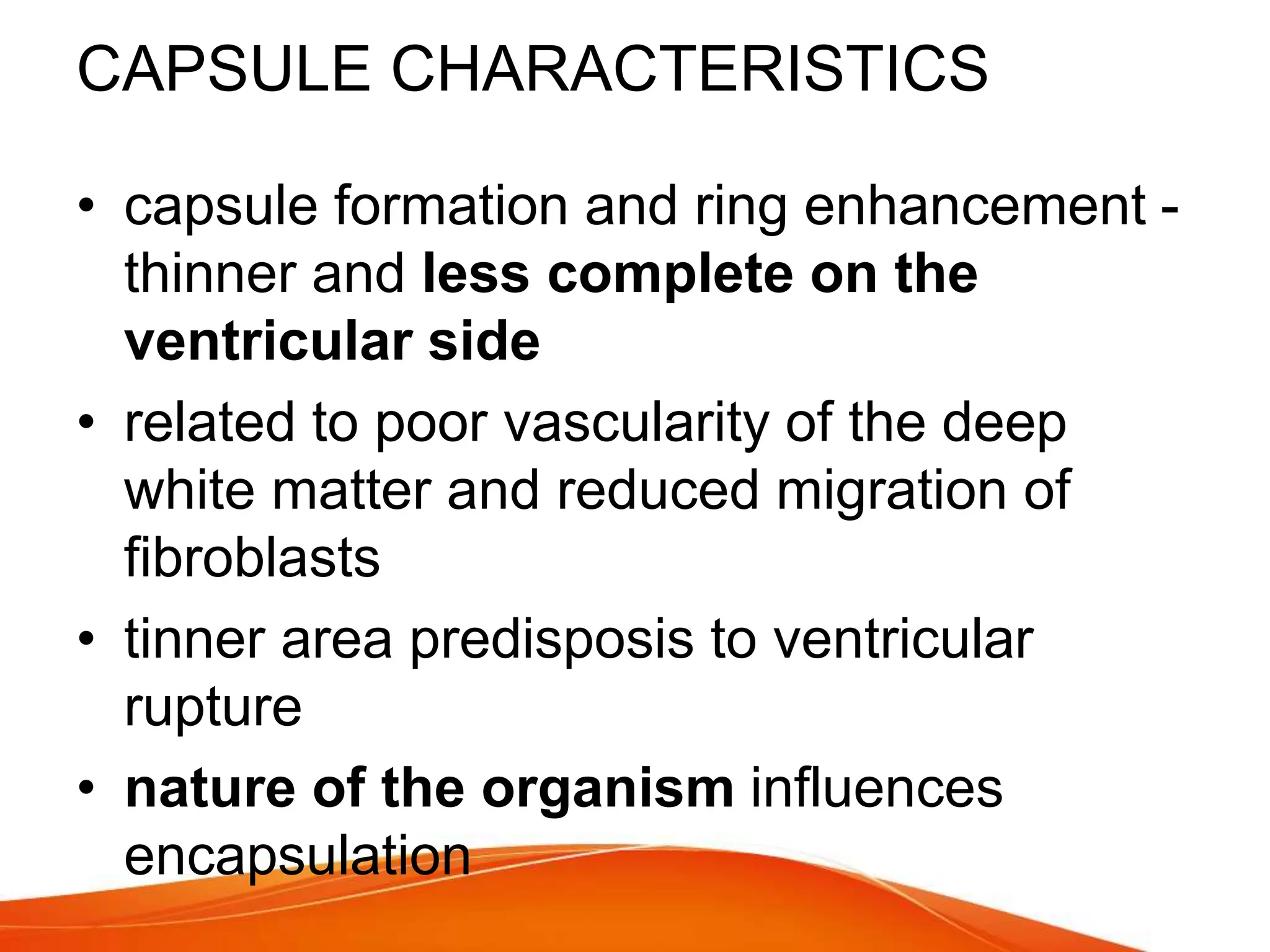
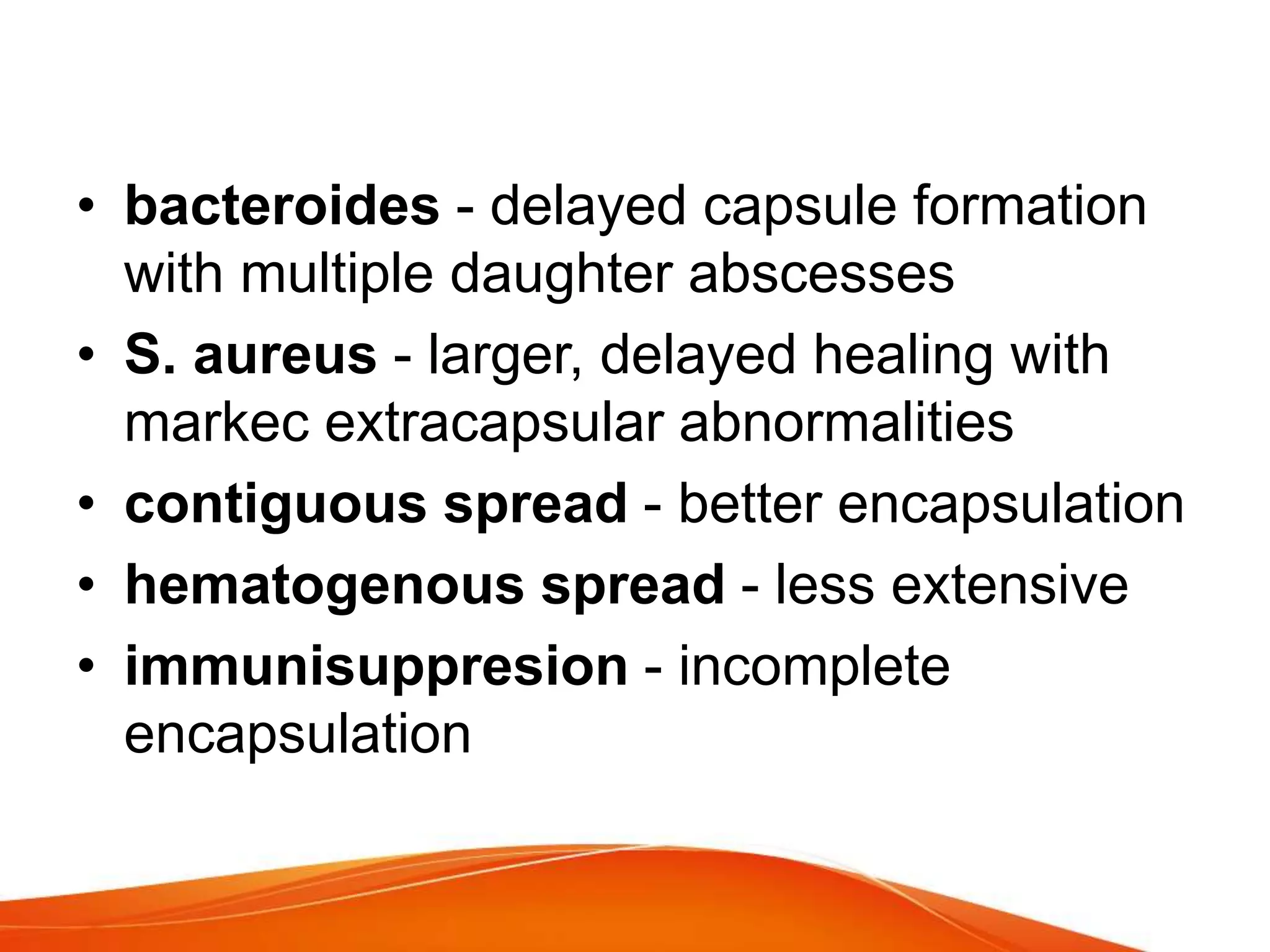
- They are focal collections of pus within the brain, most commonly caused by contiguous infections from the ear, sinuses, or mouth spreading via veins.
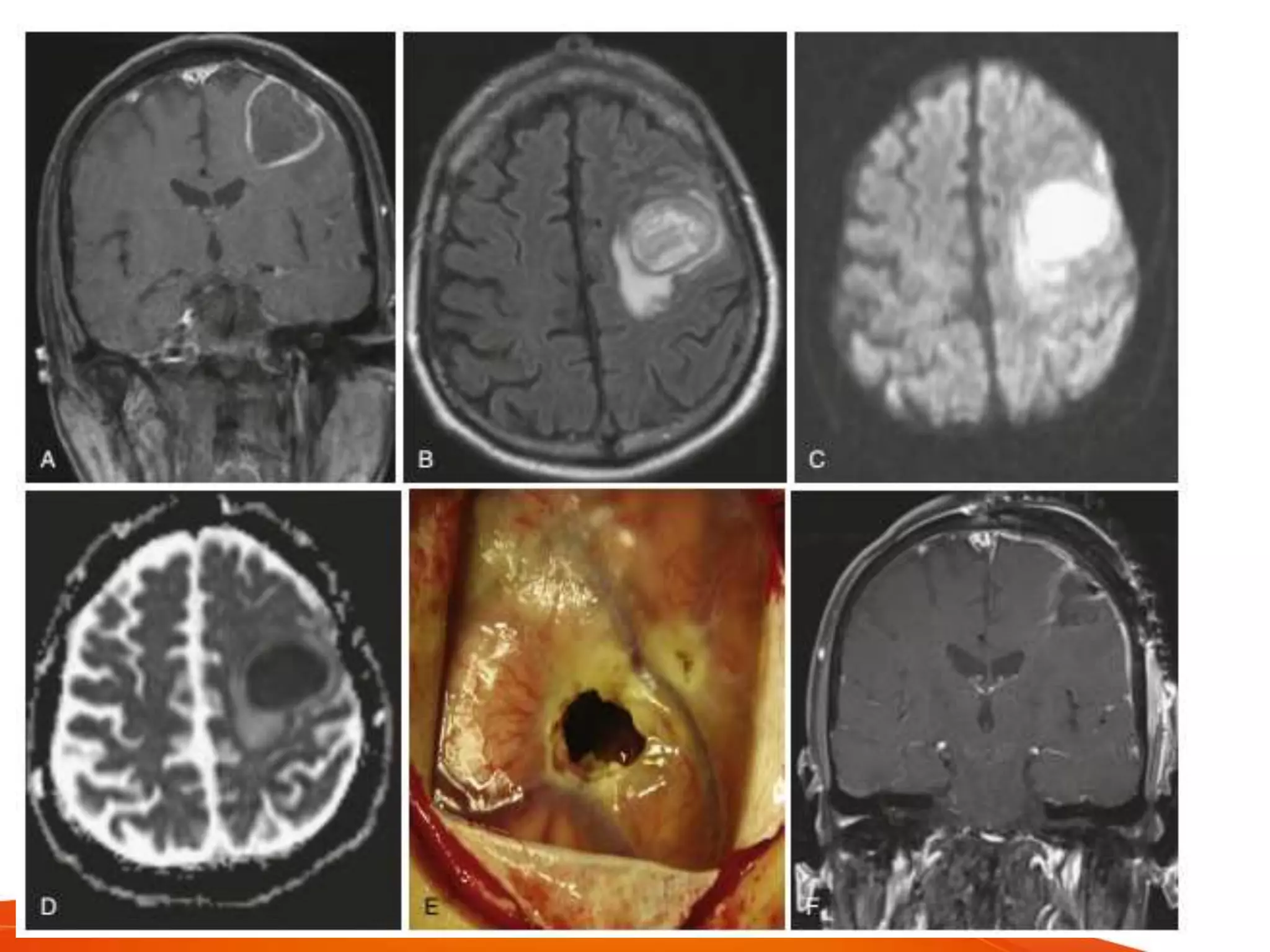
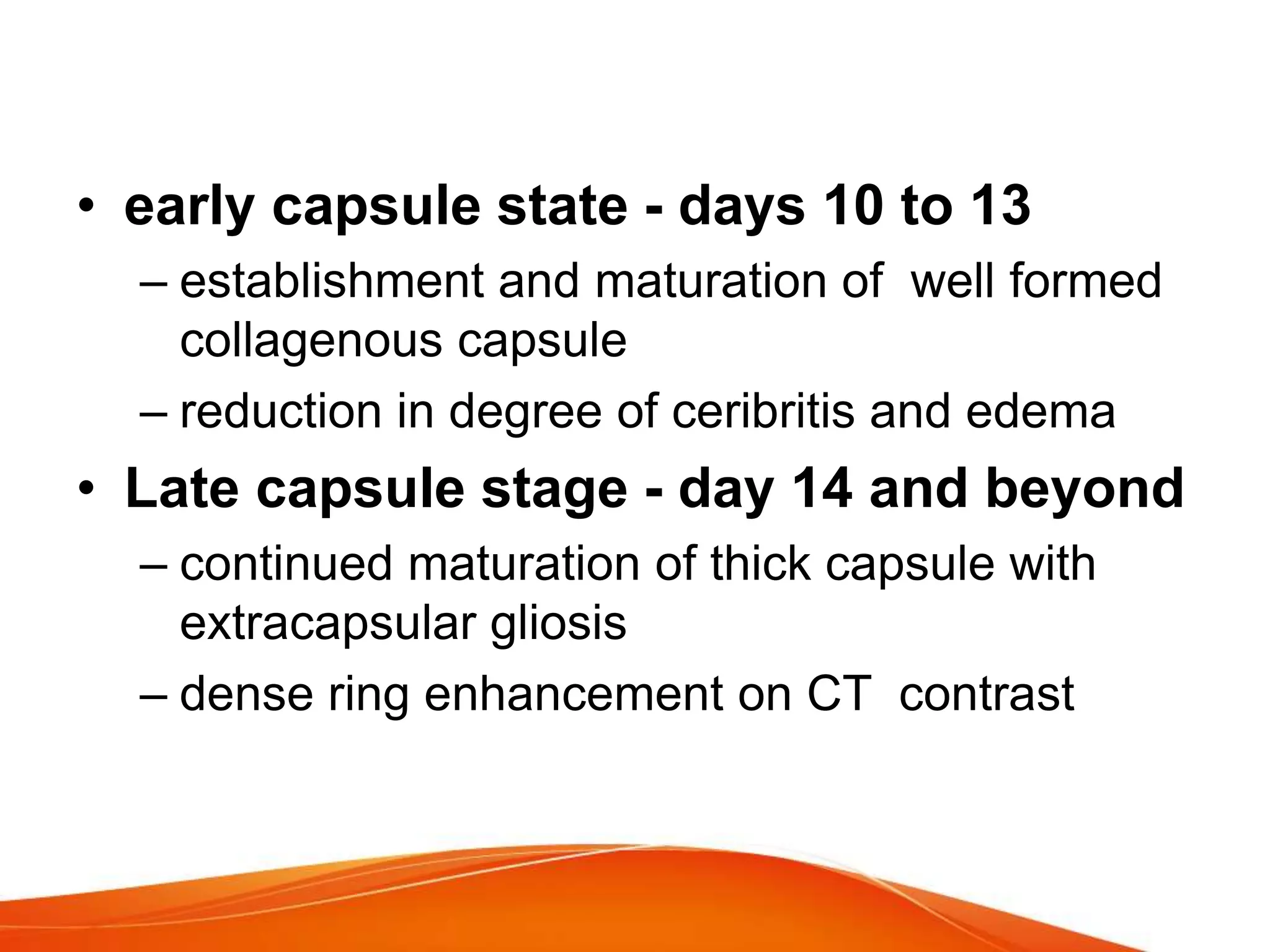
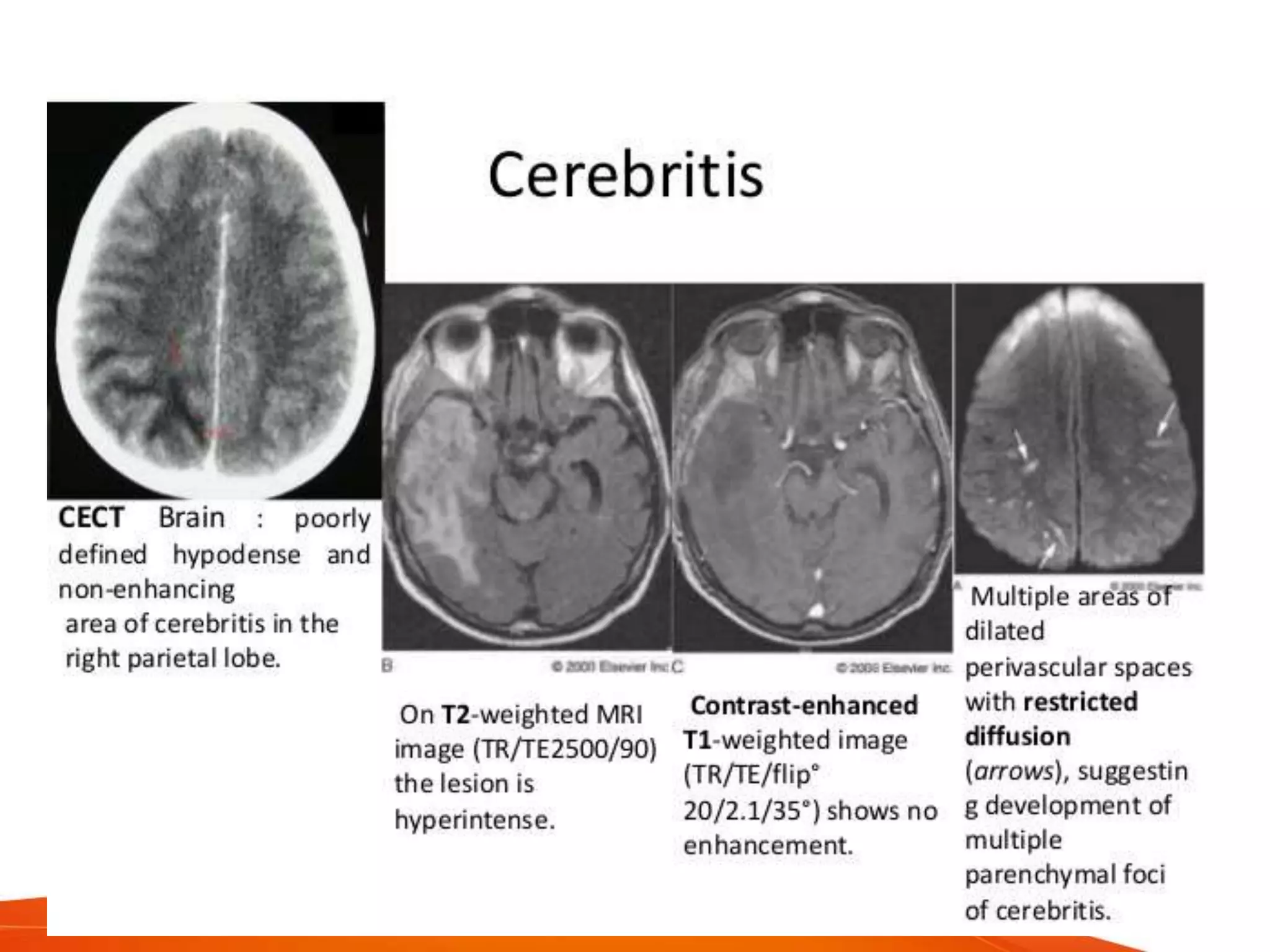
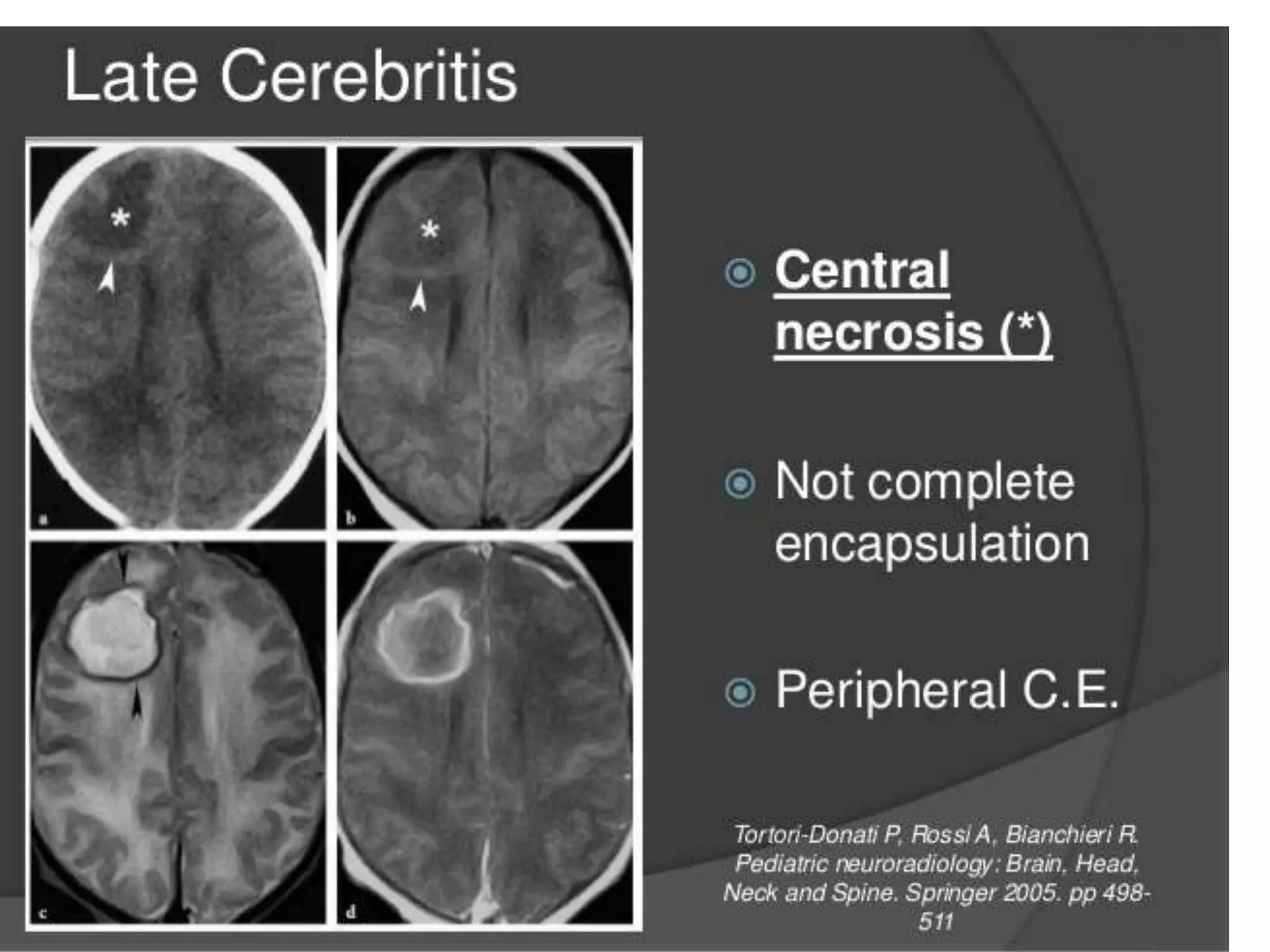
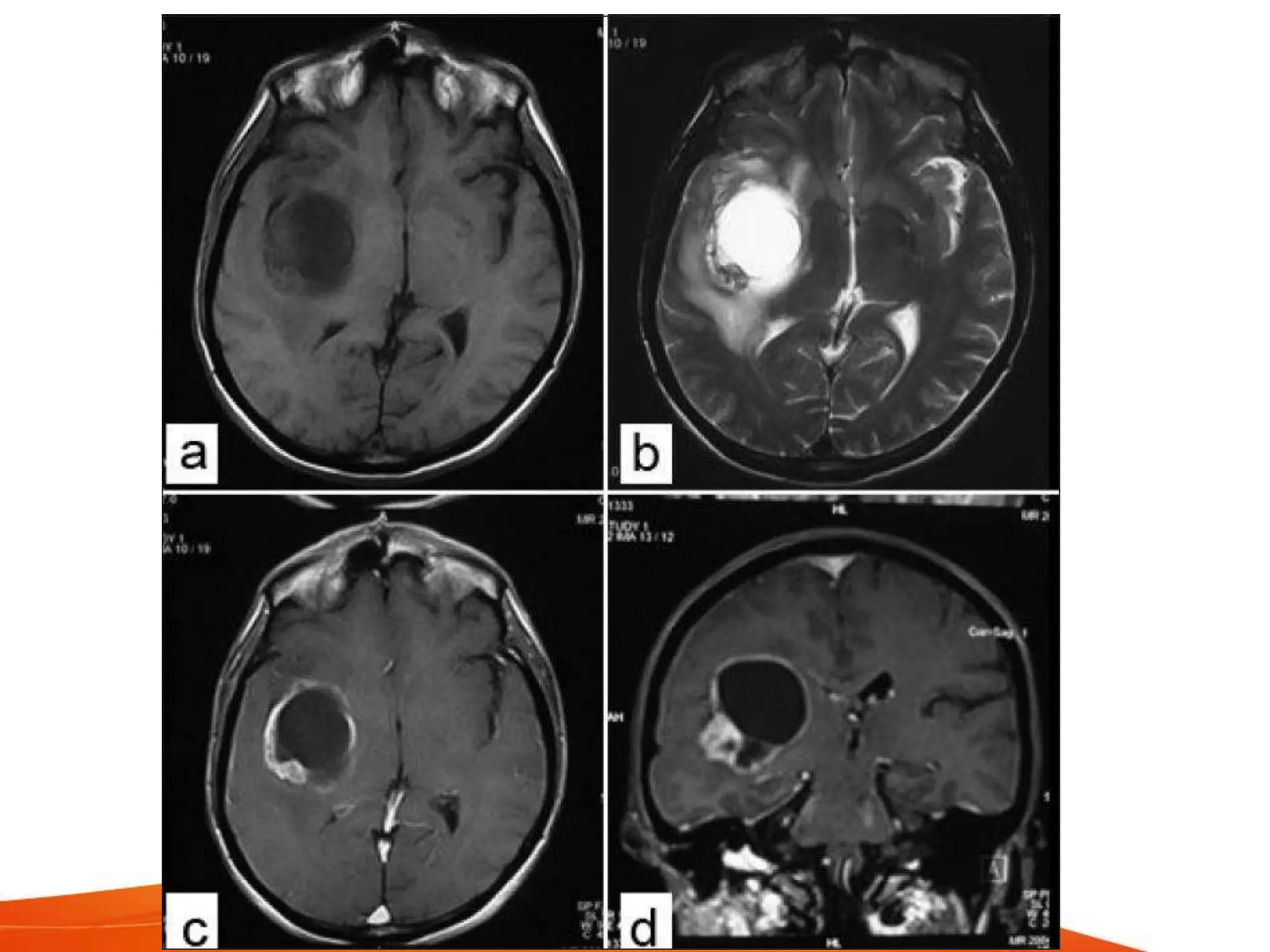
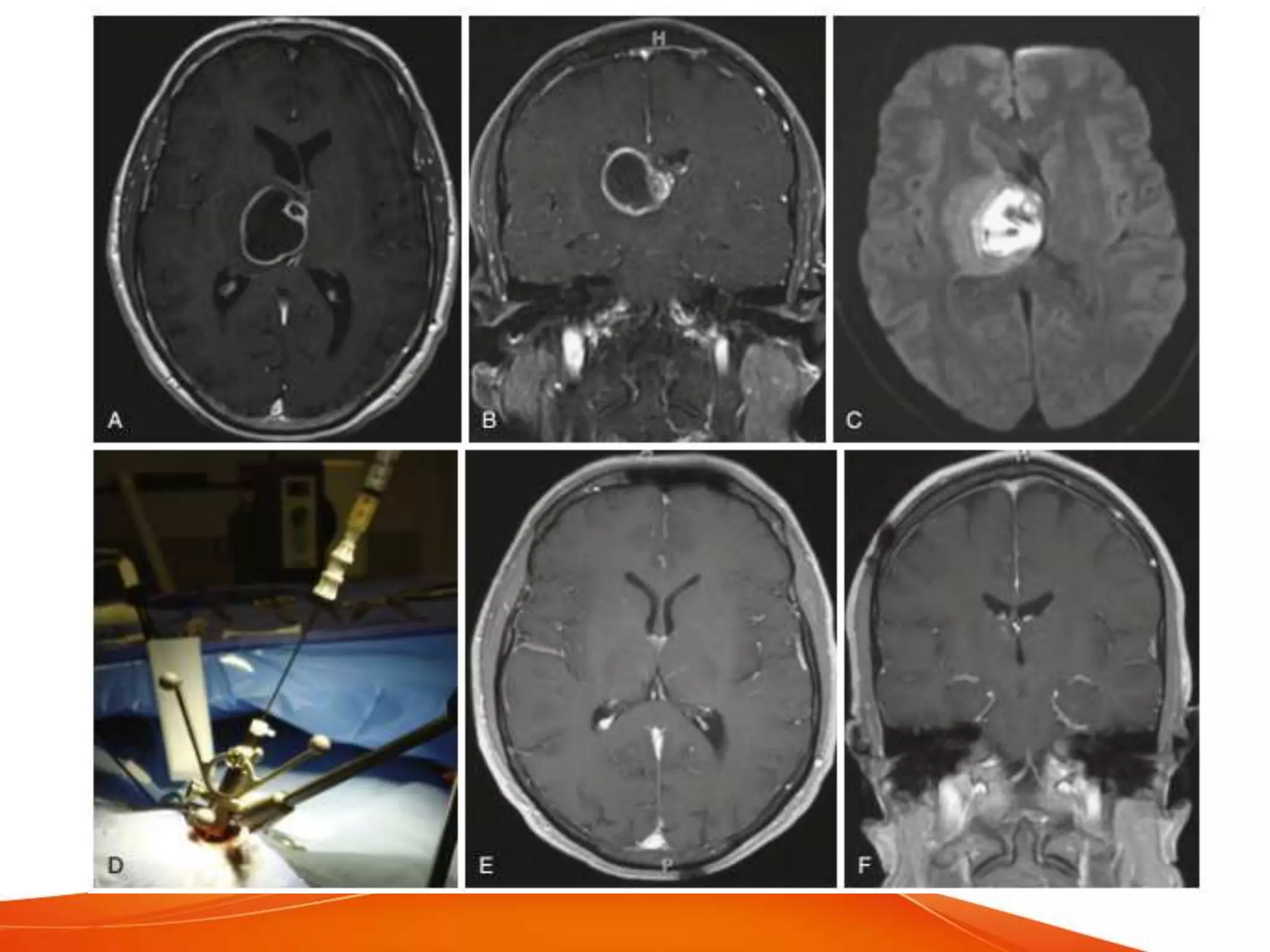
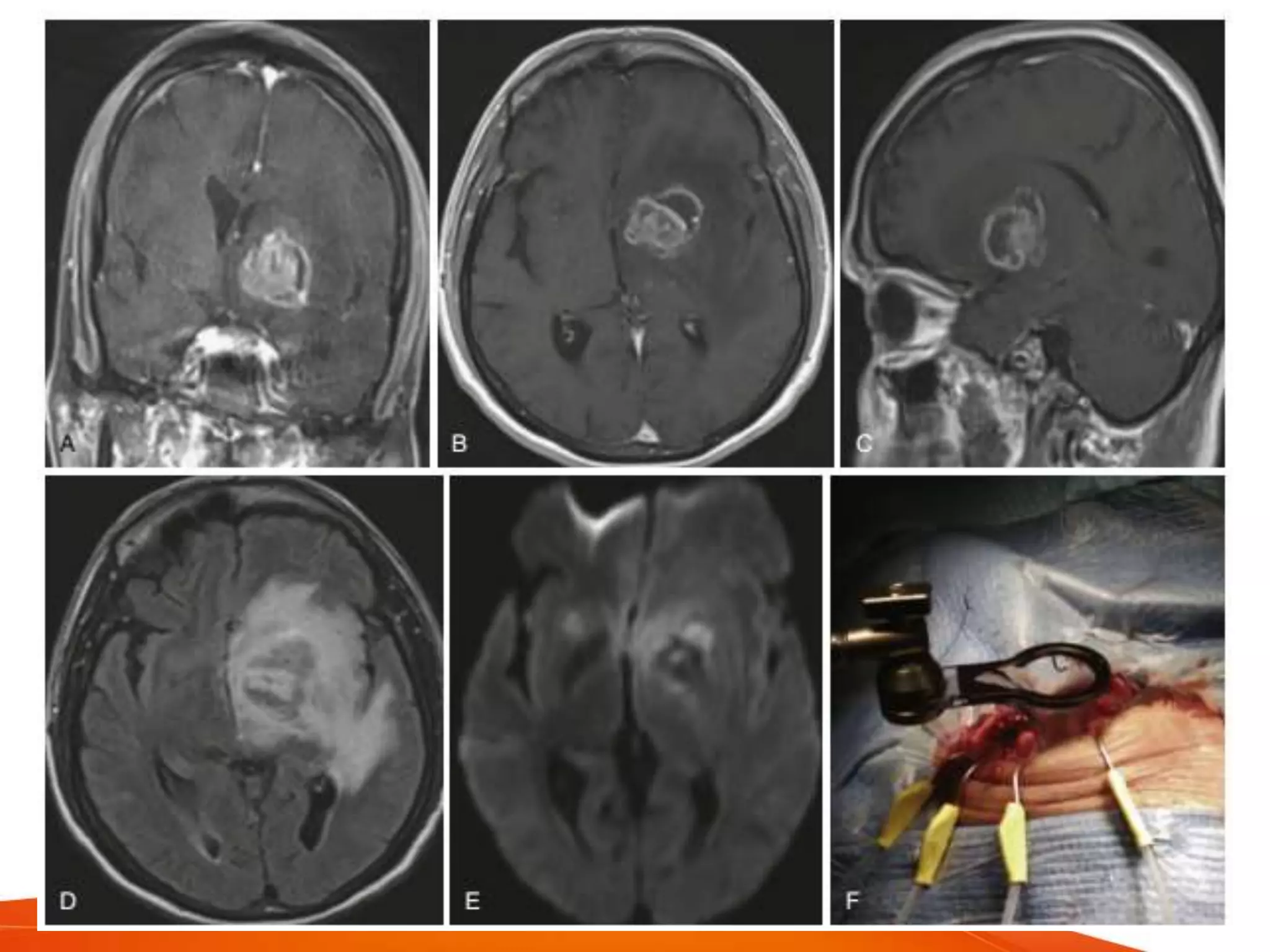
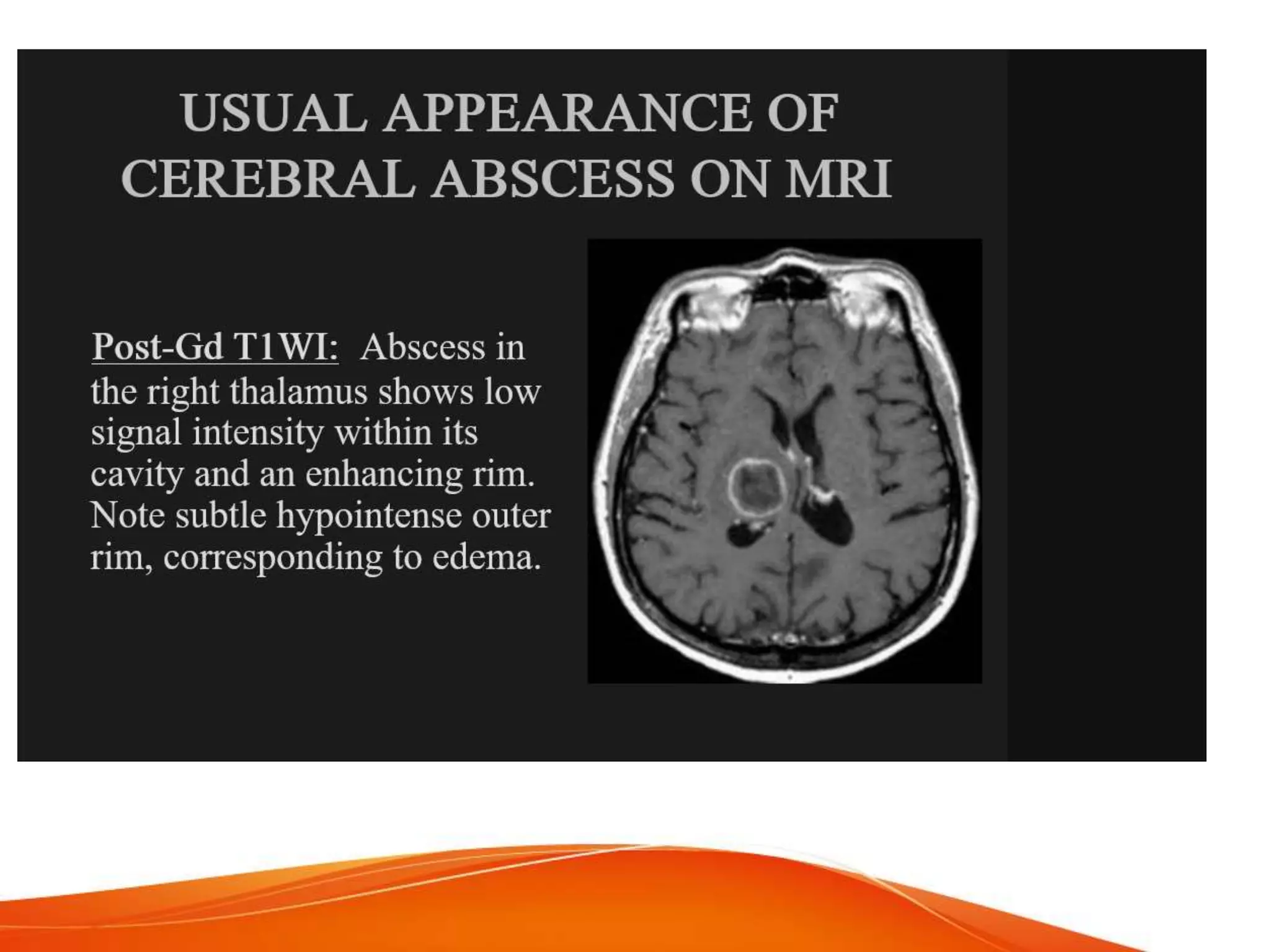
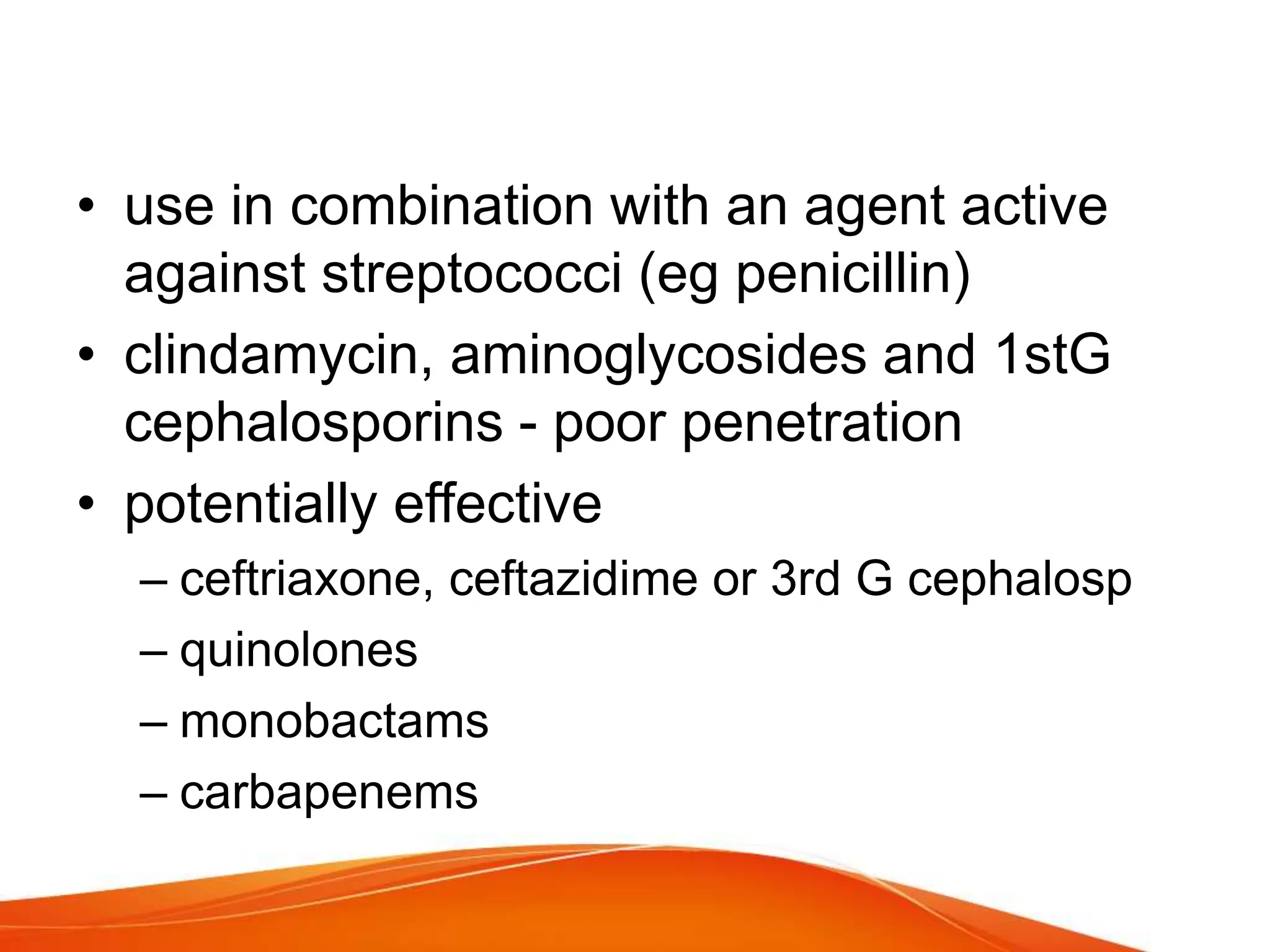
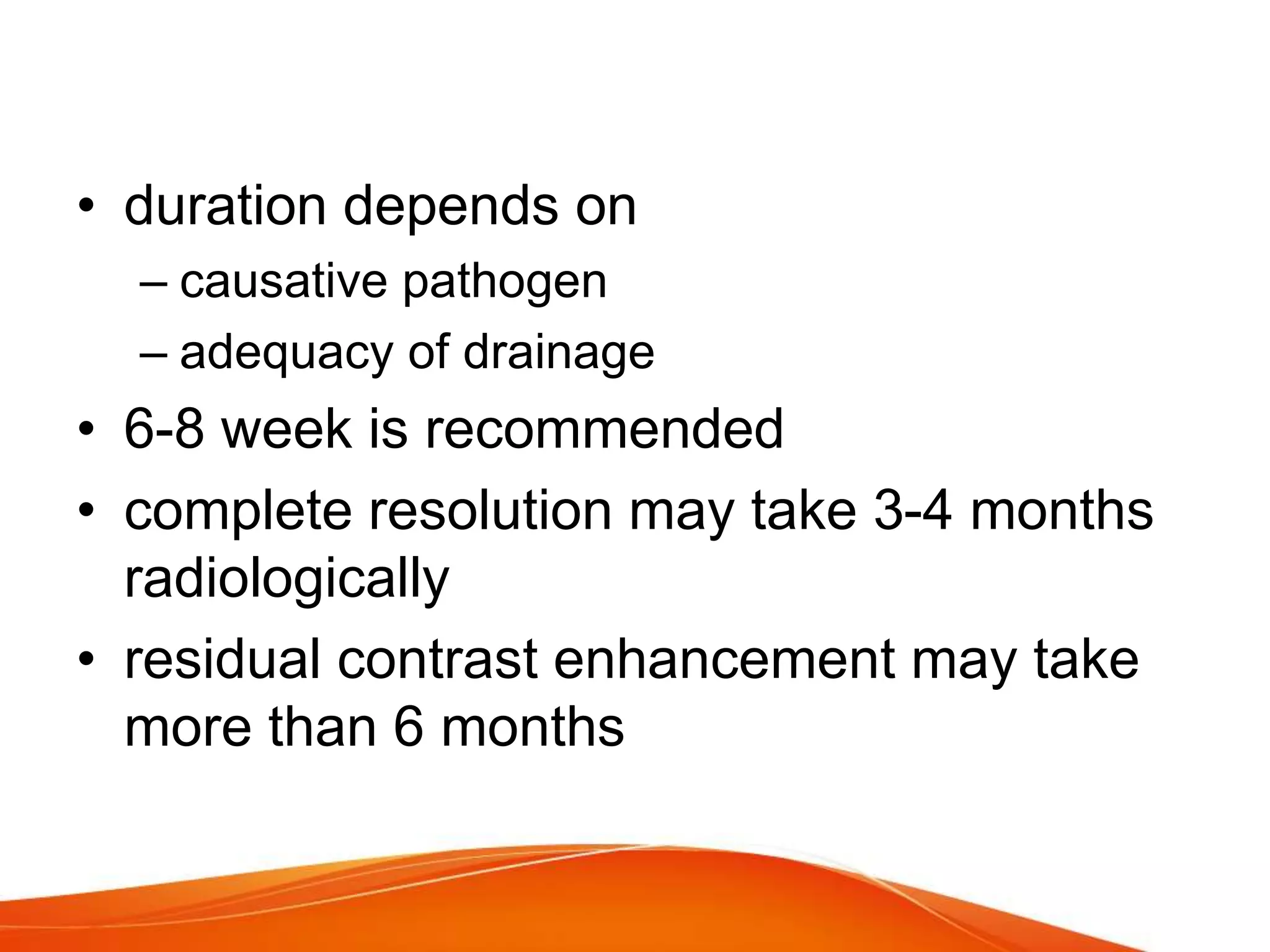
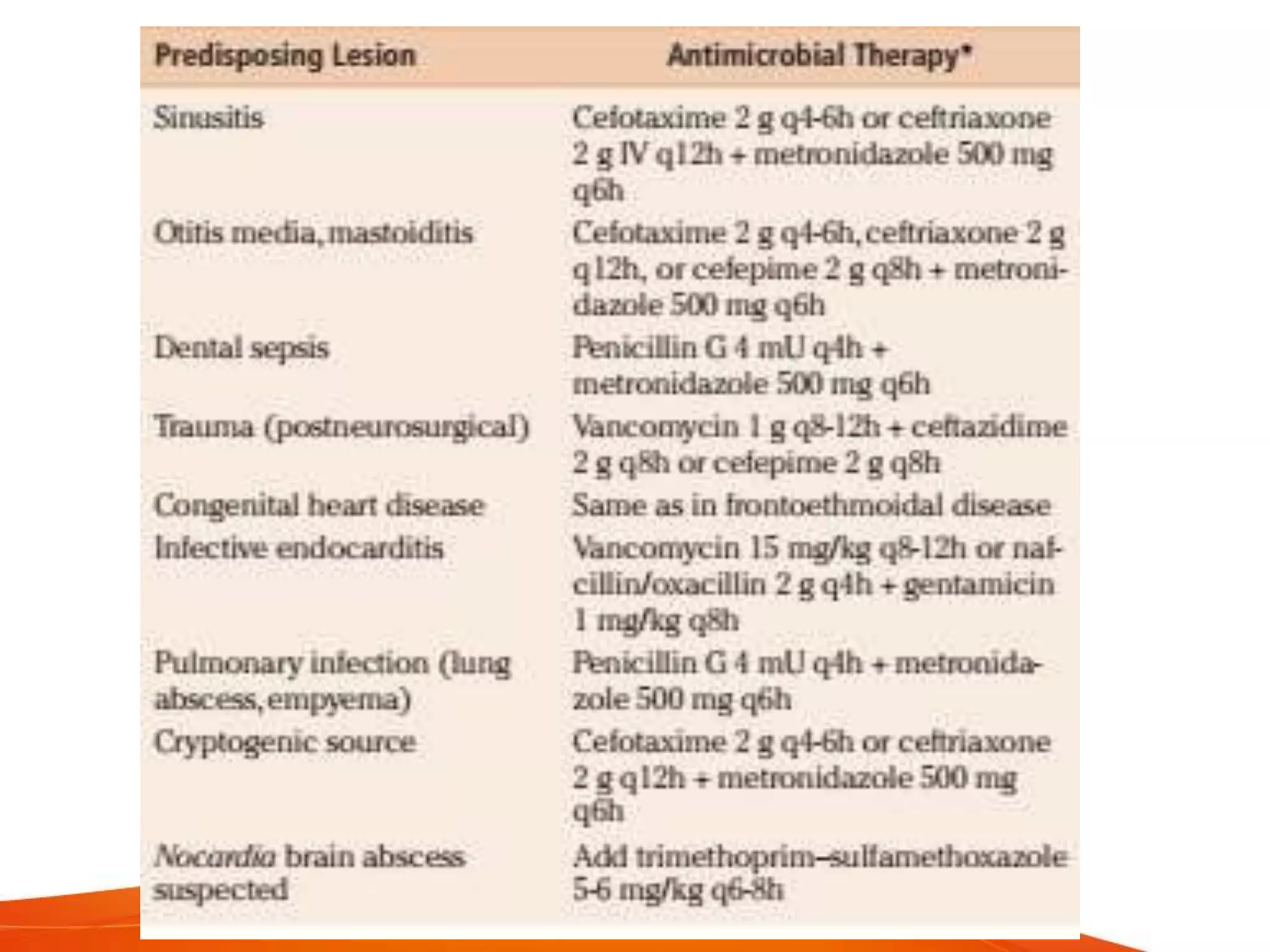
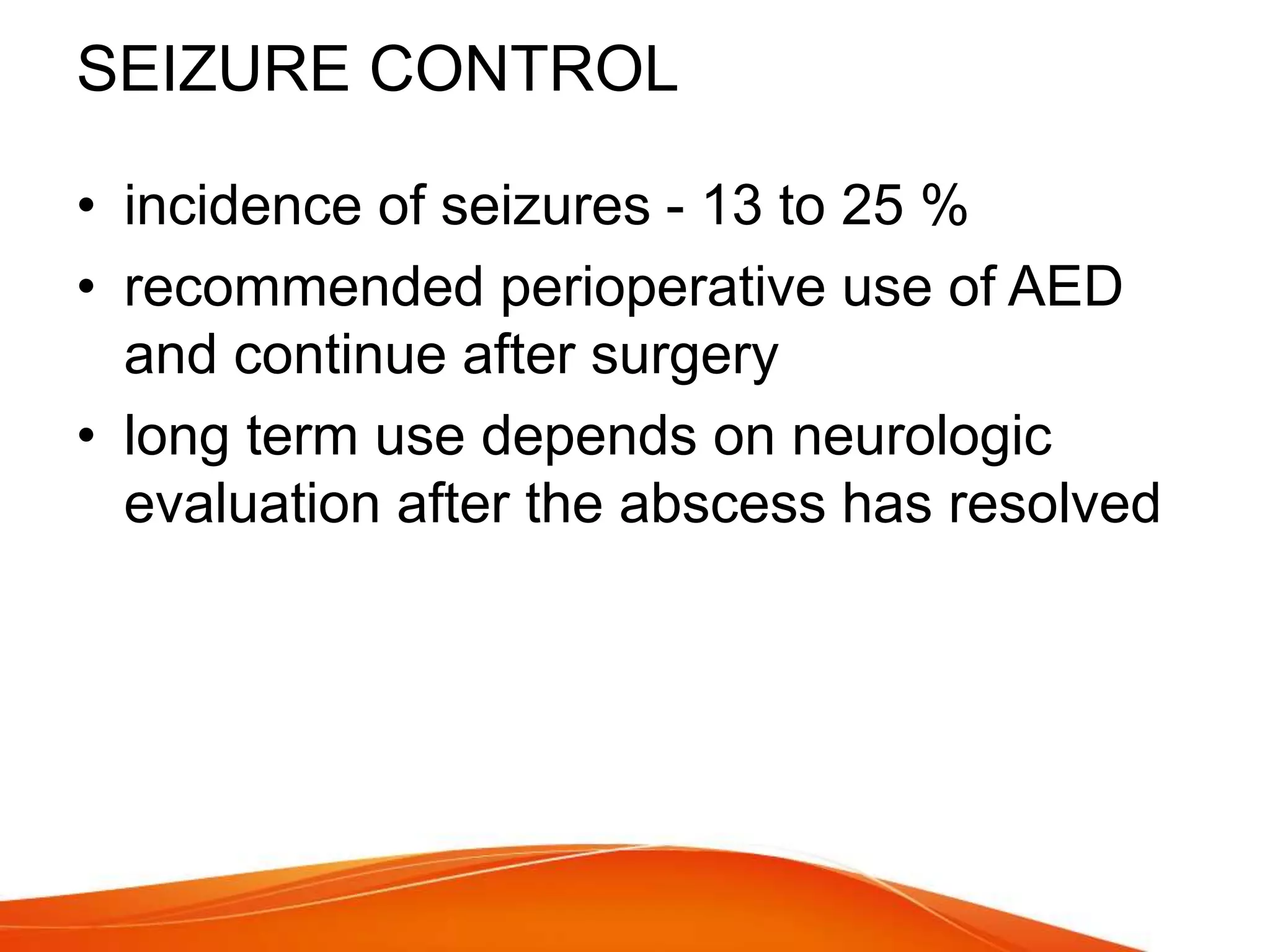
- Symptoms vary depending on size and location but often include headache, fever, and neurological deficits. Diagnosis involves CT or MRI imaging and treatment involves antibiotics plus surgical drainage for larger abscesses.