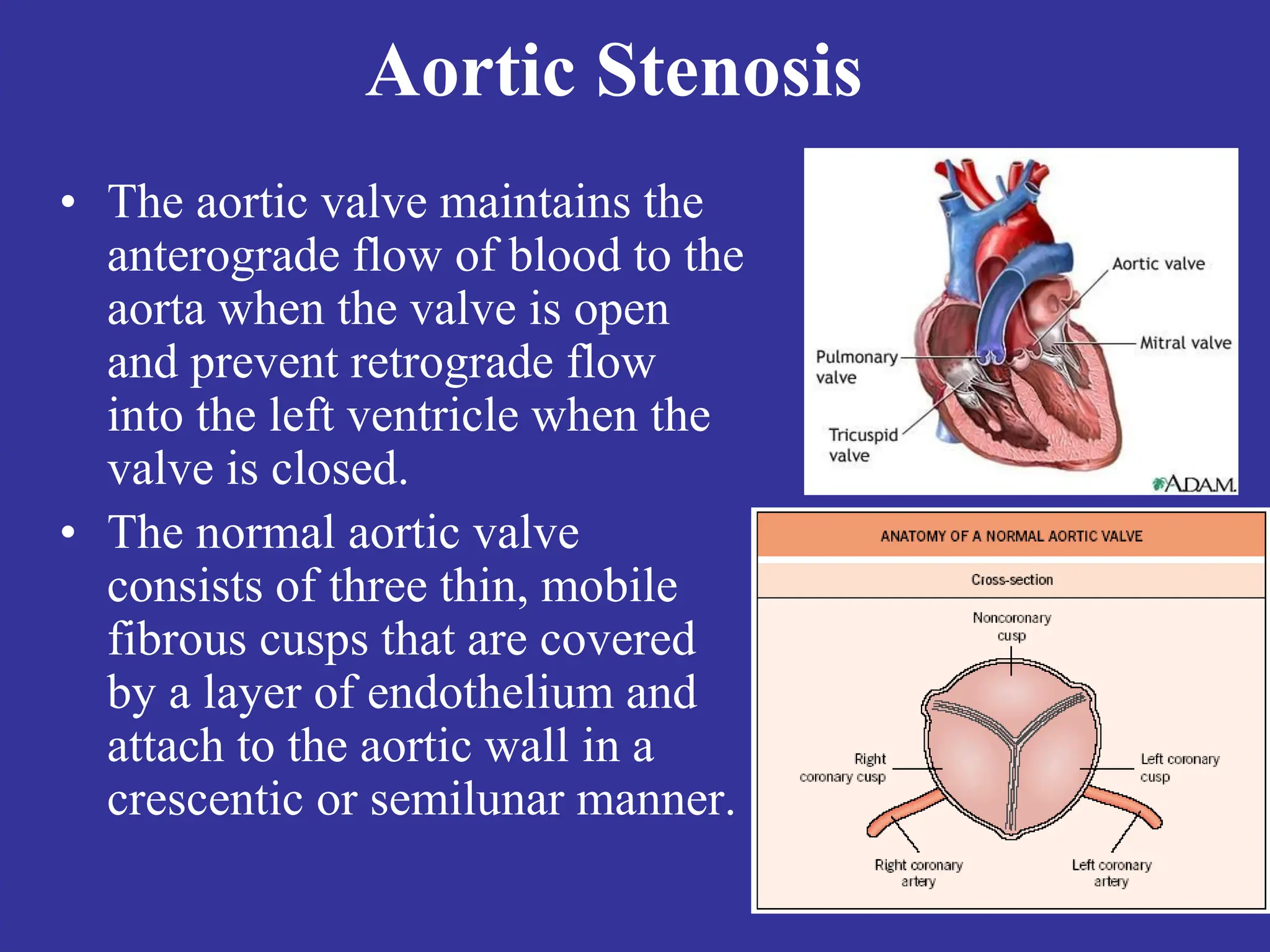
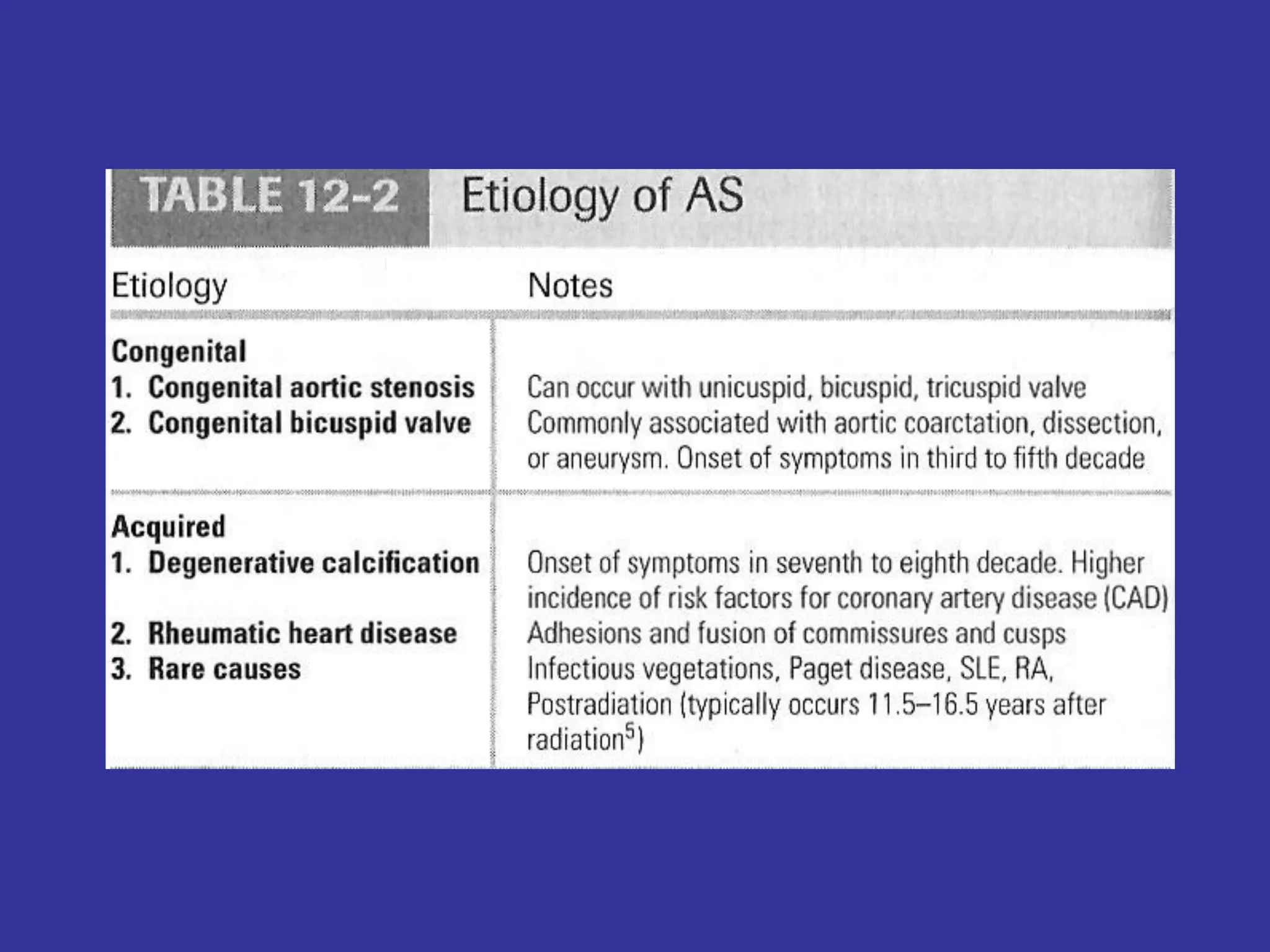
The document discusses aortic valve diseases, focusing on aortic stenosis and aortic regurgitation, including their etiology, symptoms, diagnosis, and management strategies. Aortic stenosis is prevalent, especially among the elderly, and leads to serious complications if symptomatic, requiring surgical intervention. Aortic regurgitation also presents specific diagnostic challenges, and management often involves careful monitoring and surgical options depending on symptom severity.