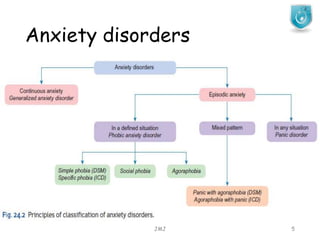
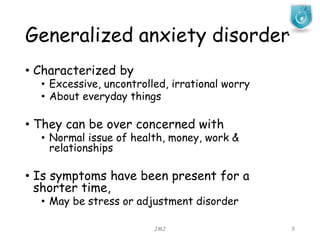
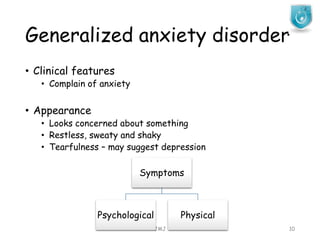
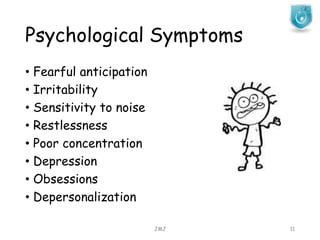
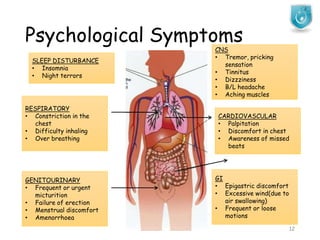
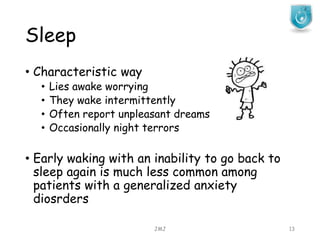
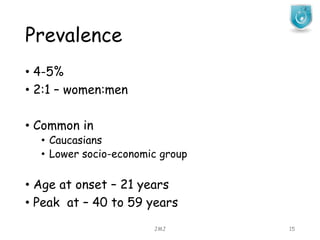
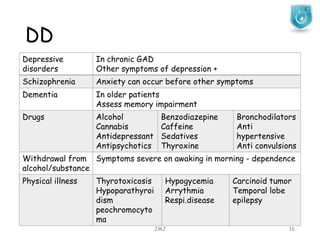
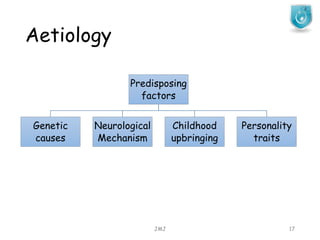
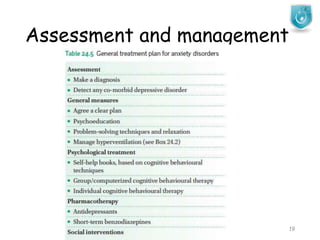
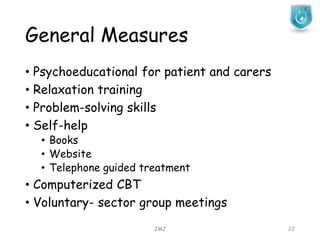
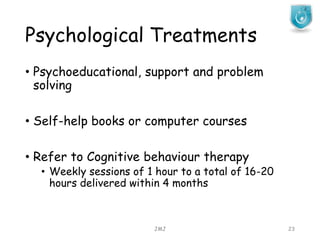
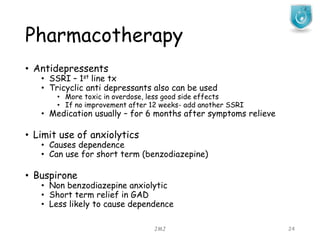
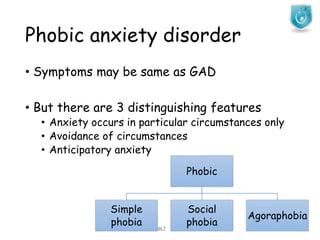
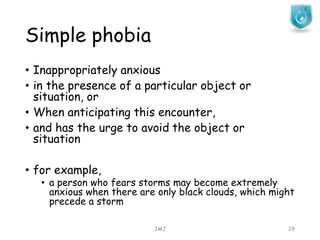
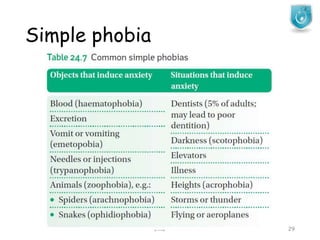
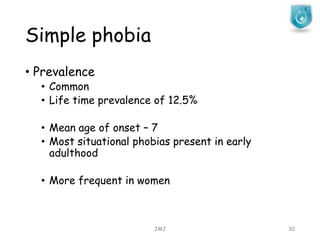
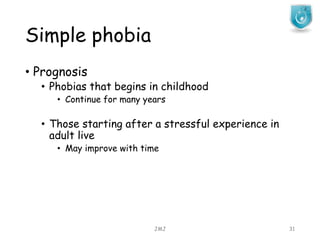
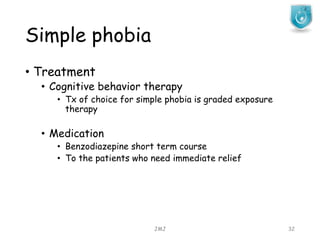
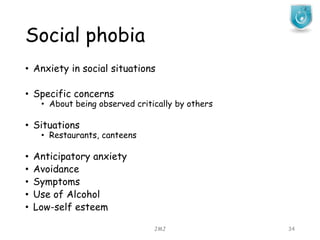
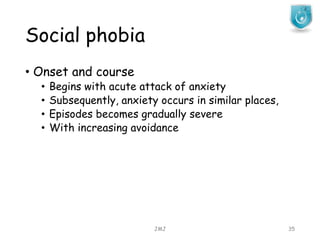
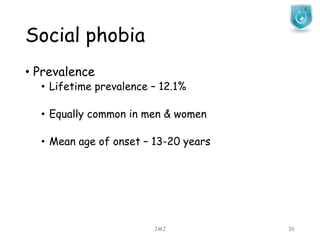
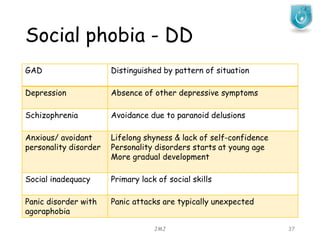
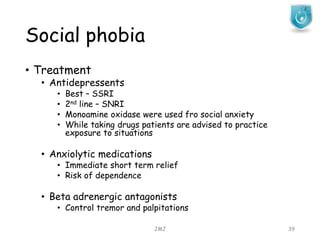
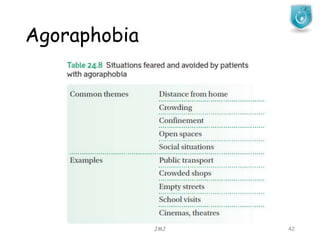
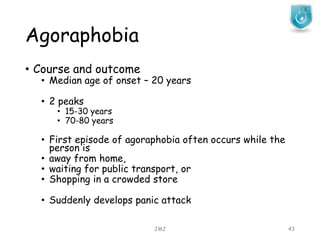
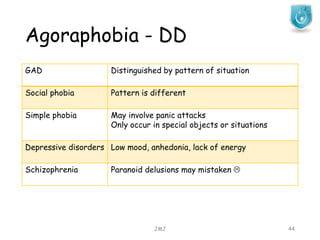
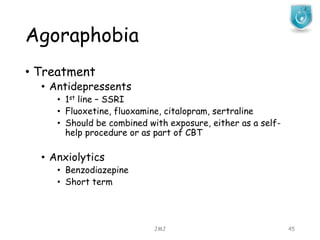
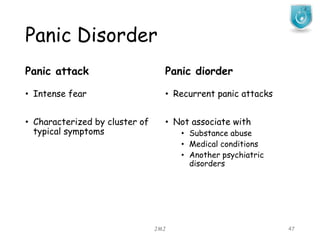
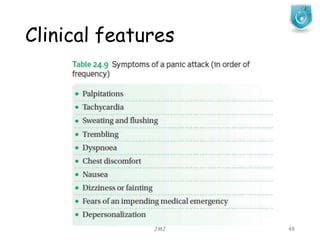
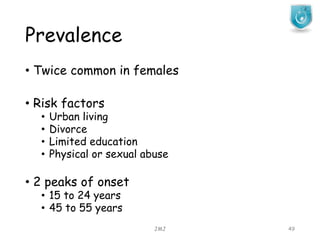
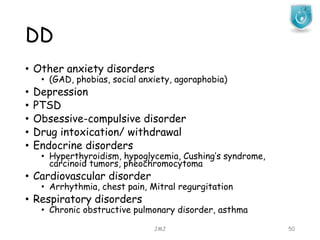
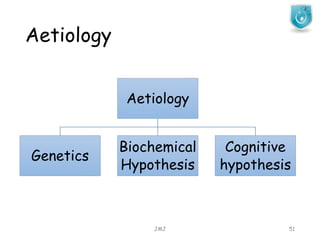
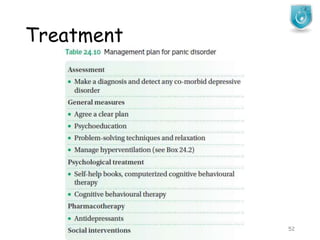
This document discusses various anxiety disorders including generalized anxiety disorder, phobic anxiety disorder, social phobia, agoraphobia, and panic disorder. It provides information on the prevalence, clinical features, course, differential diagnosis, etiology and treatment options for each disorder. The treatment options discussed include pharmacological interventions like antidepressants and anxiolytics as well as psychological therapies such as cognitive behavioral therapy and exposure therapy.