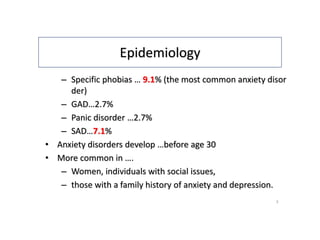
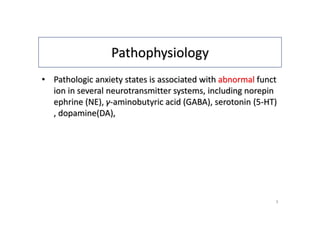
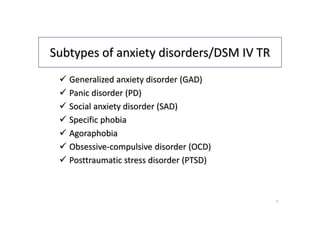
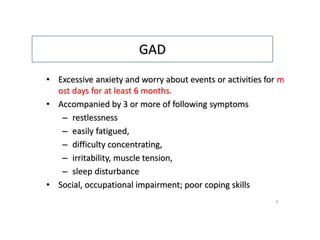
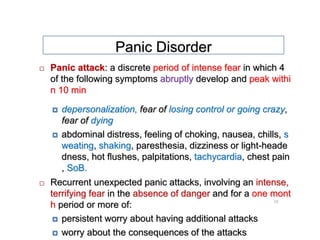
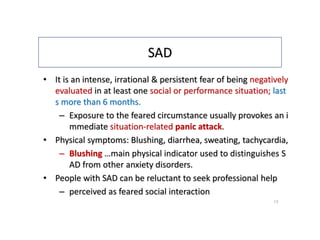
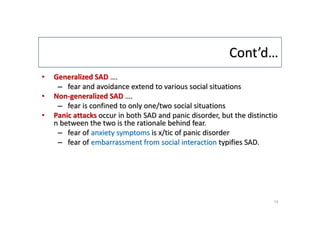
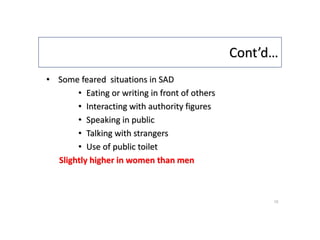
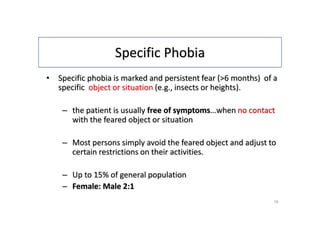
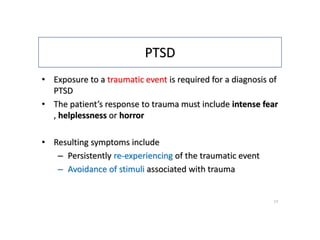
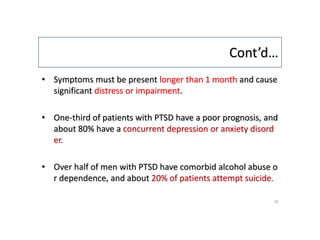
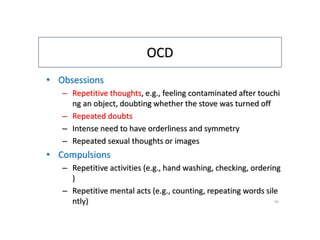
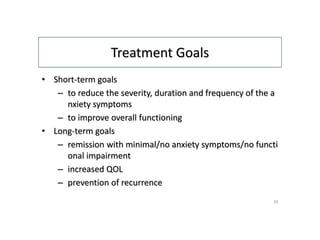
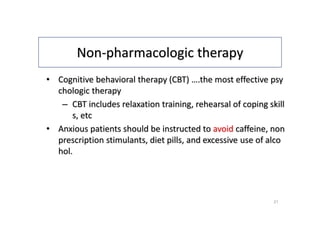
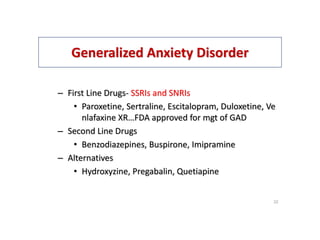
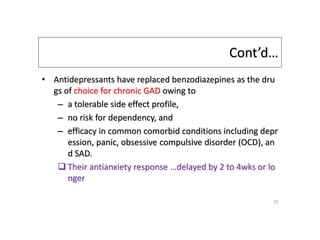
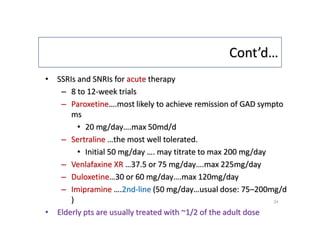
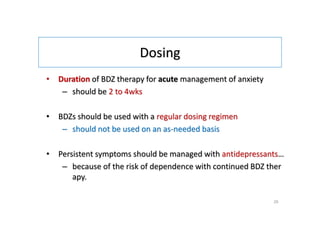
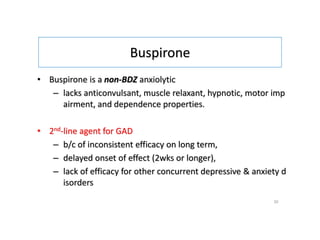
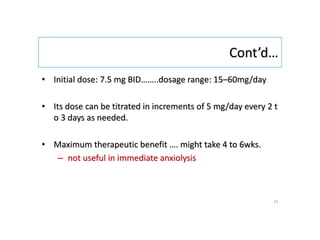
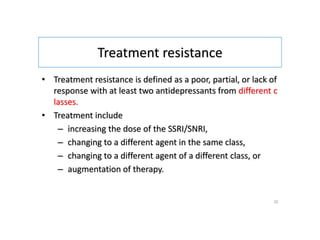
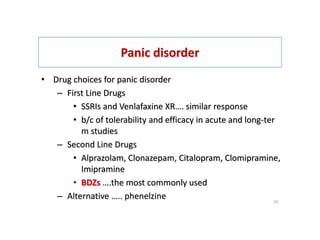
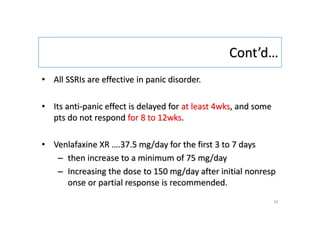
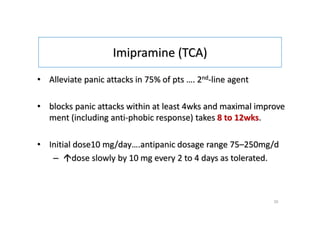
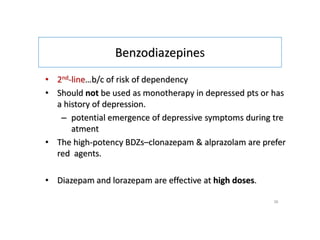
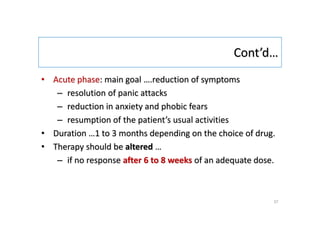
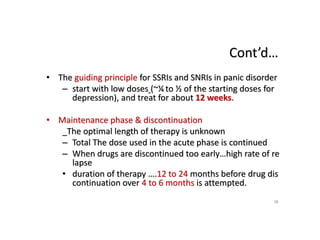
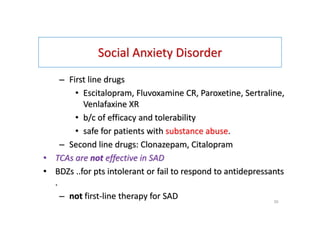
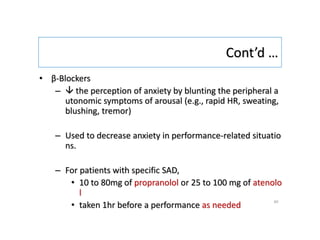
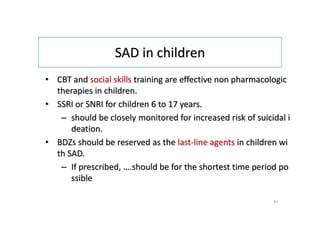
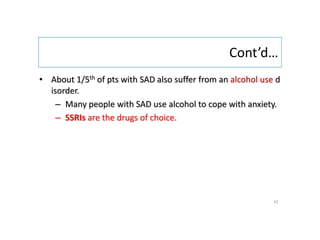
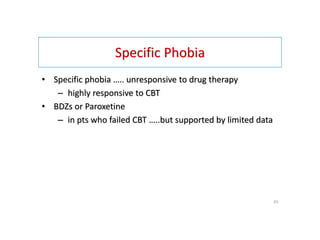
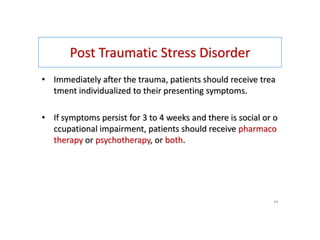
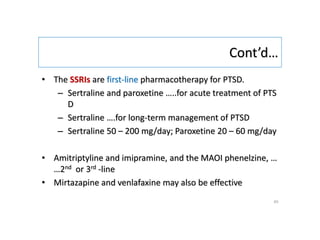
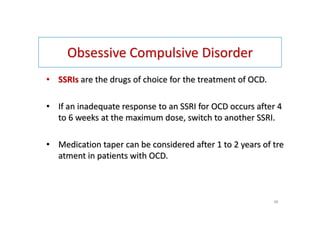
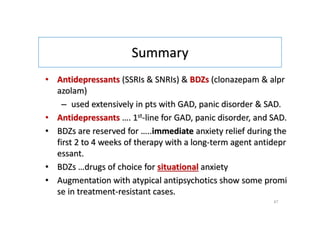
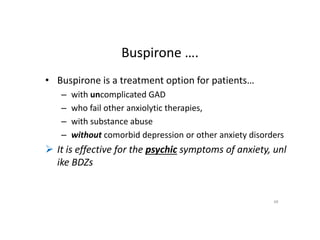
This document provides an overview of anxiety disorders, including their epidemiology, etiology, pathophysiology, clinical presentation, subtypes, and treatment approaches. It discusses the characteristics and management of several specific anxiety disorders, including generalized anxiety disorder, panic disorder, social anxiety disorder, specific phobia, and post-traumatic stress disorder. Pharmacologic and non-pharmacologic treatment options are described.