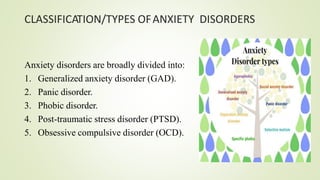
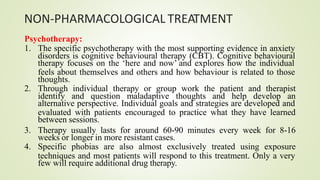
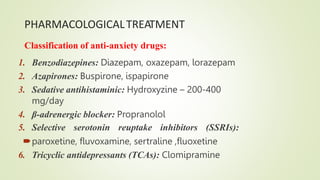
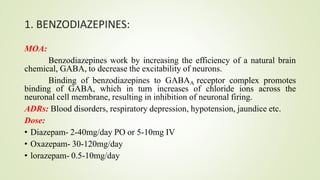
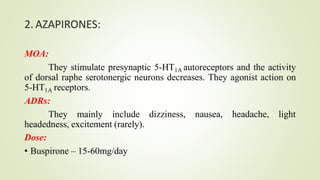
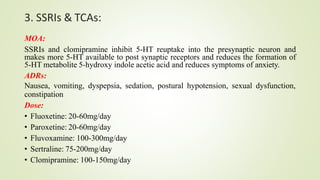
Anxiety disorders are characterized by excessive and persistent feelings of apprehension. They are common, affecting up to 13% of people in the US. Genetic and environmental factors can contribute to their development. Anxiety has physical, behavioral, and cognitive symptoms like increased heart rate, avoidance behaviors, and worrying thoughts. Treatment involves psychotherapy like cognitive behavioral therapy and medication. Common medications are benzodiazepines, SSRIs, and other antidepressants, which work to balance brain chemicals like GABA and serotonin. Both pharmacological and non-pharmacological approaches are usually needed to manage anxiety disorders long-term.