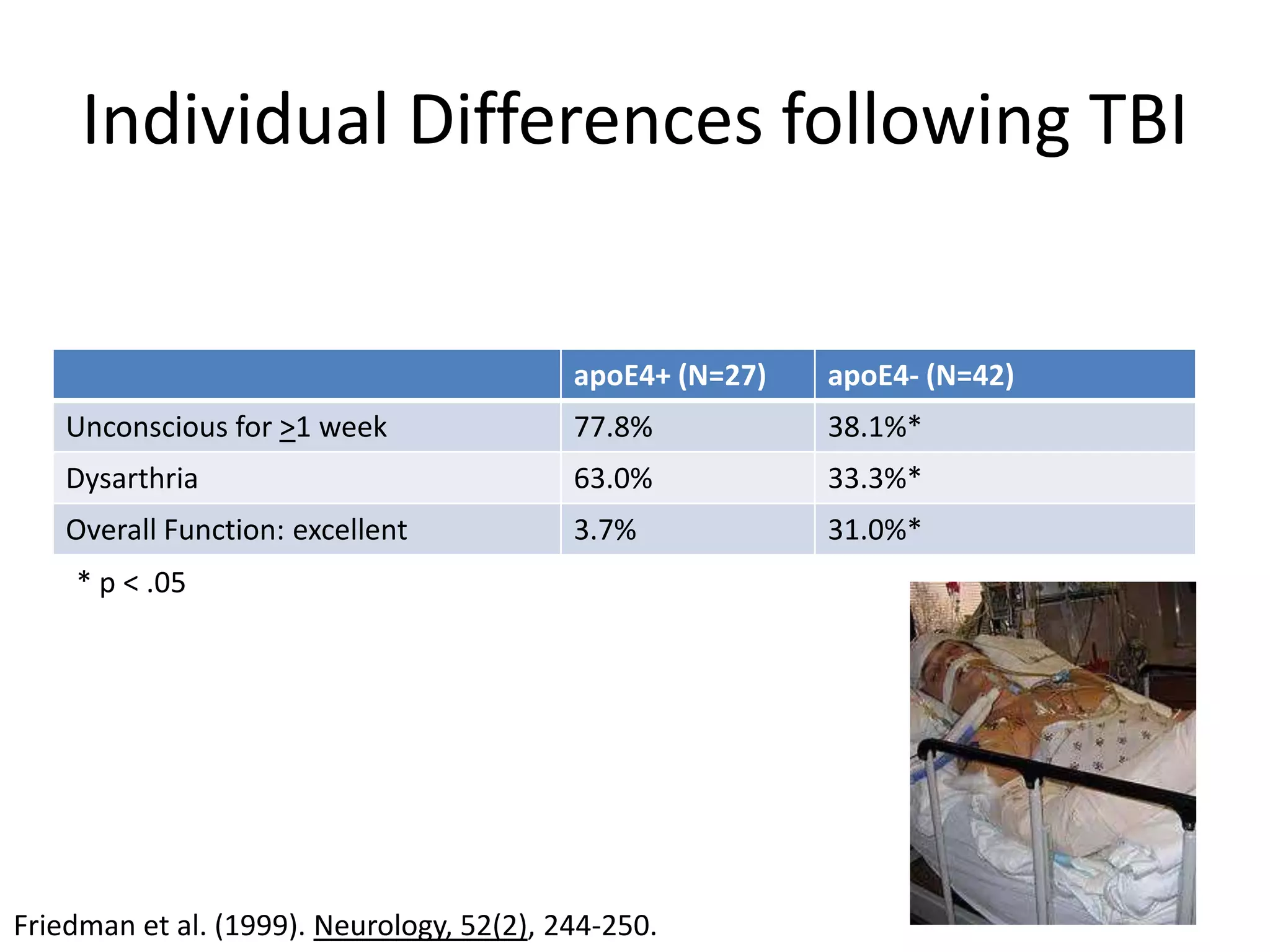
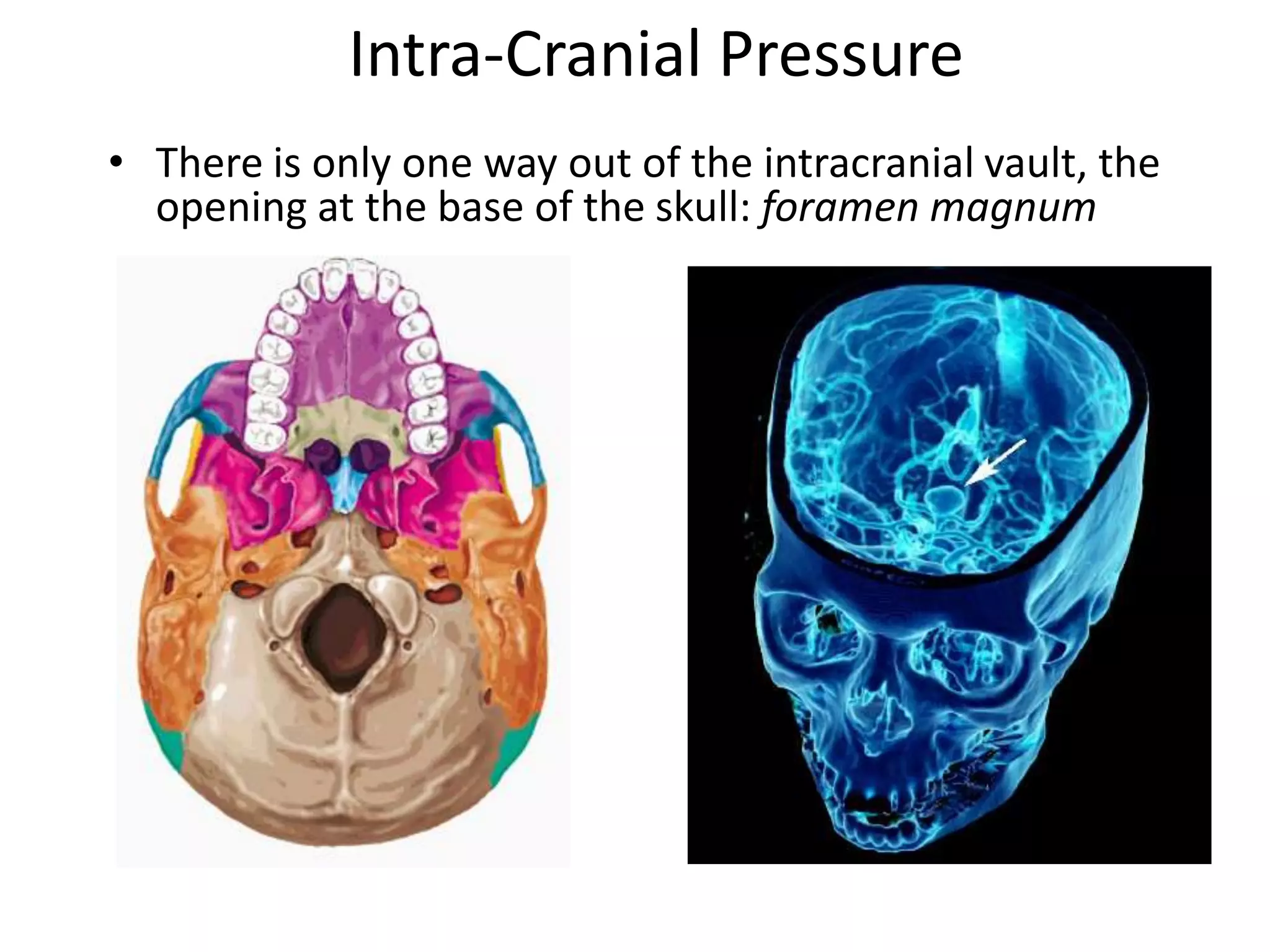
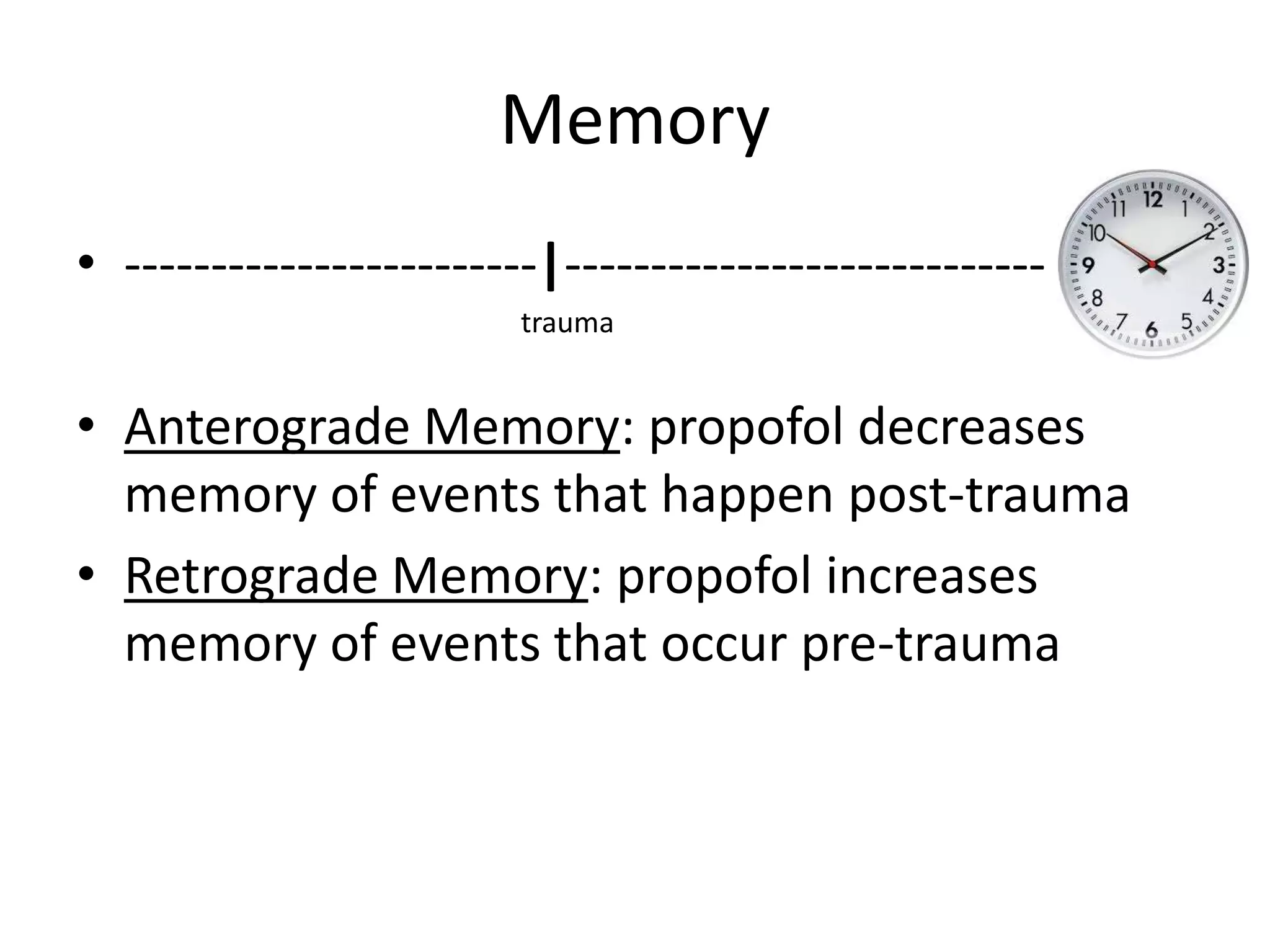
The document discusses pharmacotherapies for traumatic brain injury (TBI) that pharmacy students should know, including their mechanisms, efficacy, and adverse effects. It highlights the distinction between primary injury at impact and secondary injury which develops thereafter due to factors like hypotension and increased intracranial pressure. Treatment options like mannitol and barbiturates are evaluated, but the evidence for their effectiveness in TBI management remains inconclusive.