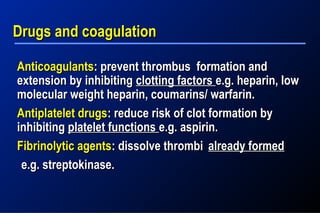
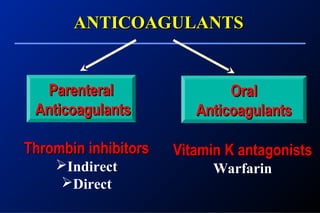
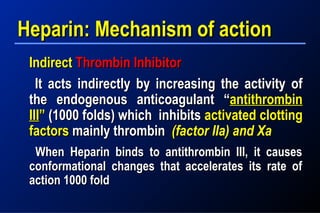
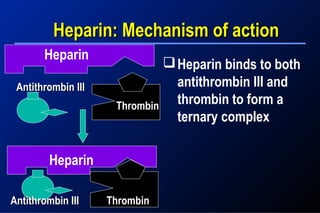
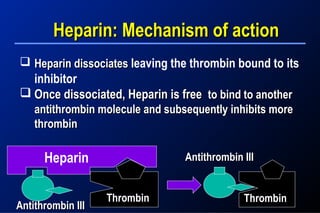
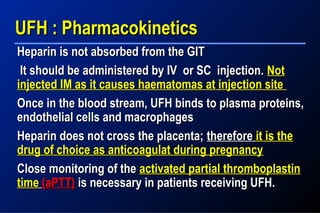
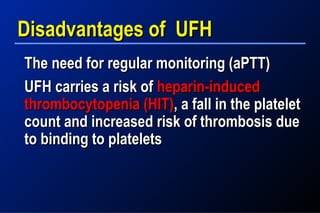
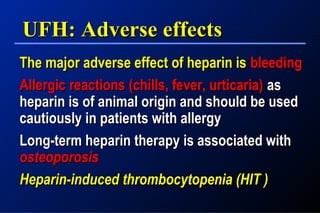
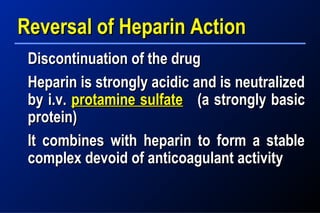
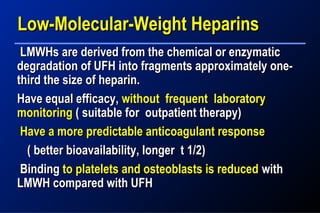
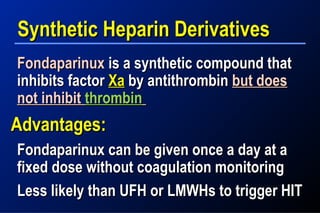
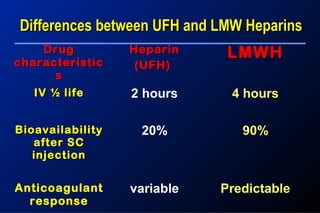
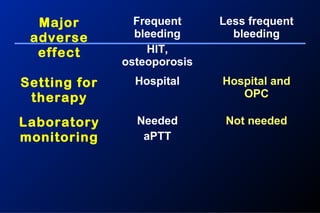
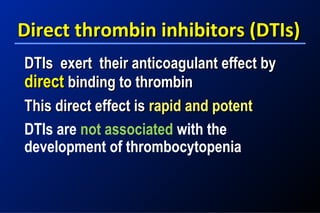
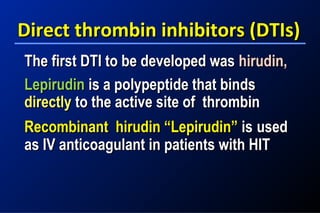
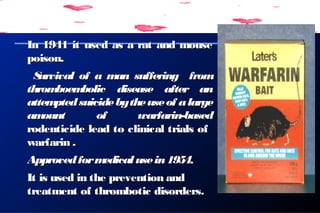
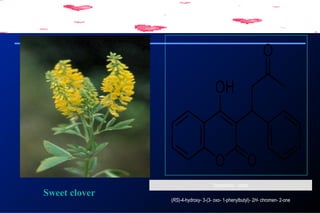
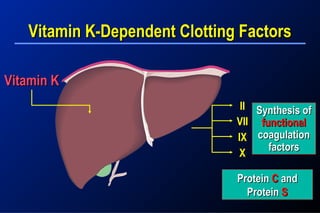
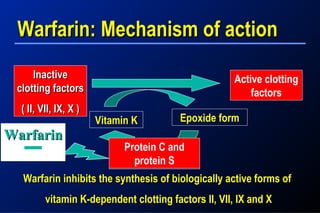
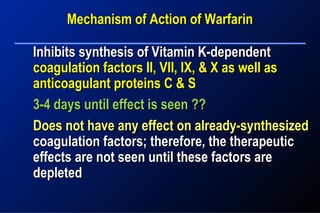
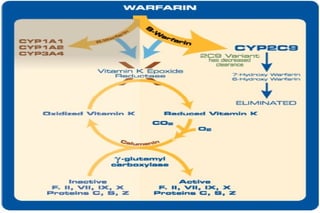
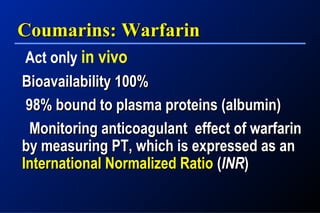
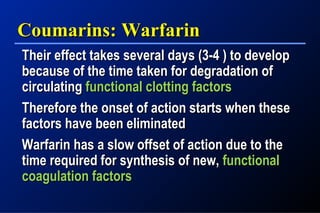
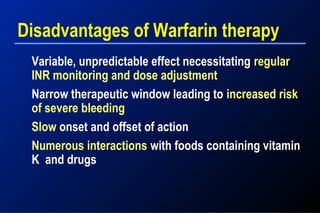
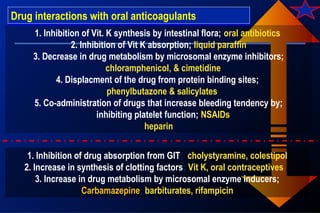
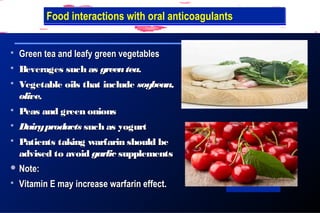
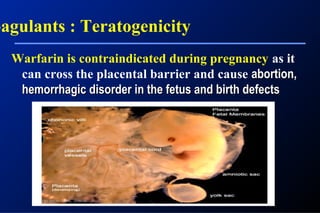
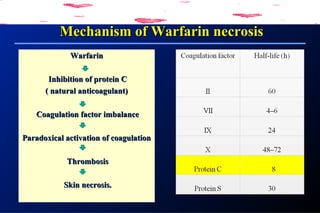
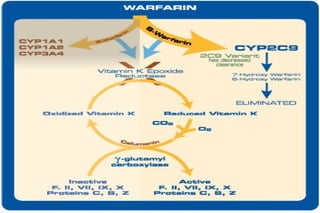
This document discusses different types of anticoagulants and antiplatelet drugs including their mechanisms of action, indications, and side effects. It covers parenteral anticoagulants like heparin and low molecular weight heparins. It also discusses oral anticoagulants like warfarin which is a vitamin K antagonist that inhibits the synthesis of clotting factors. The document compares the properties of different anticoagulants and notes their interactions with foods and other drugs.