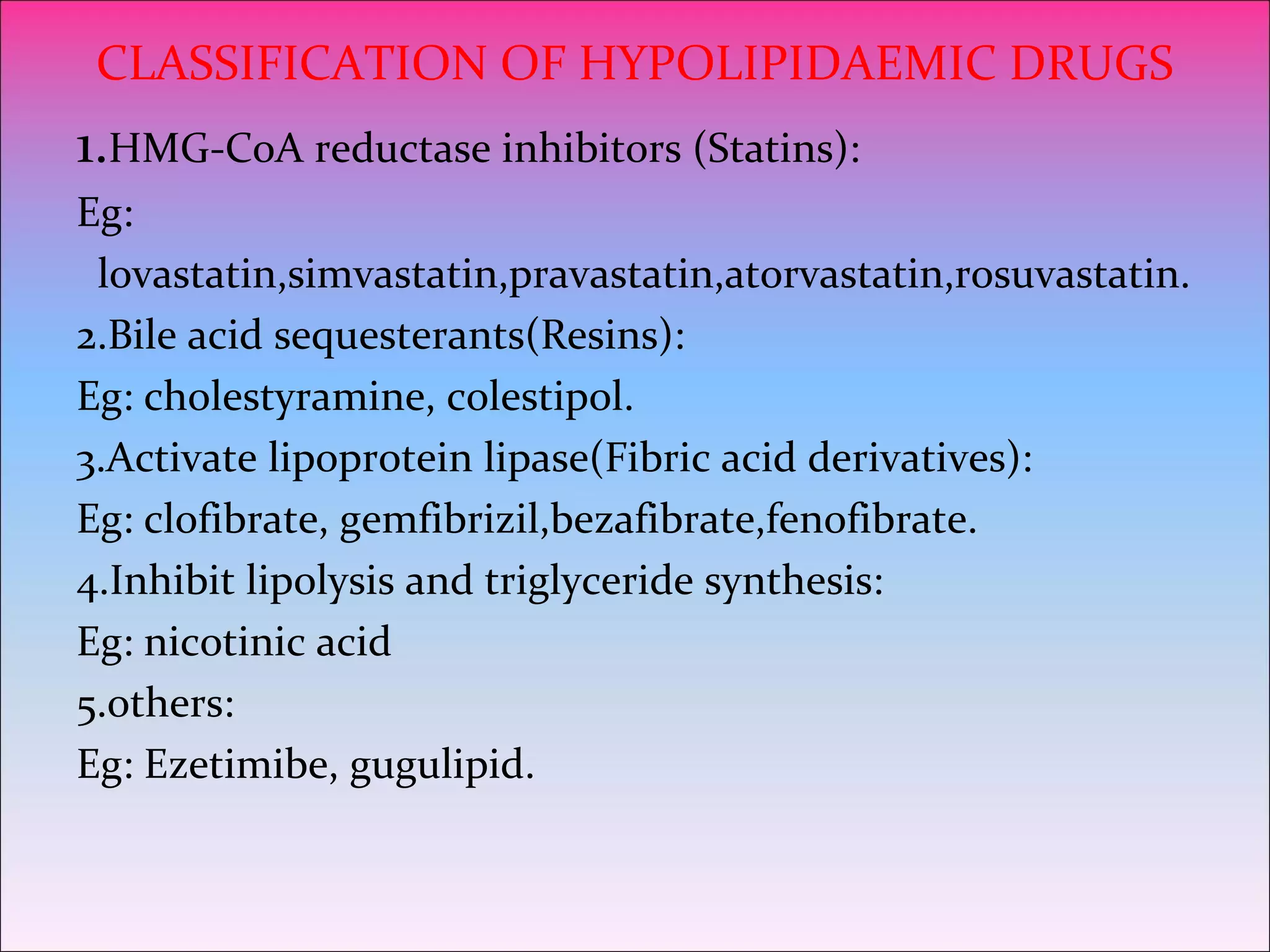
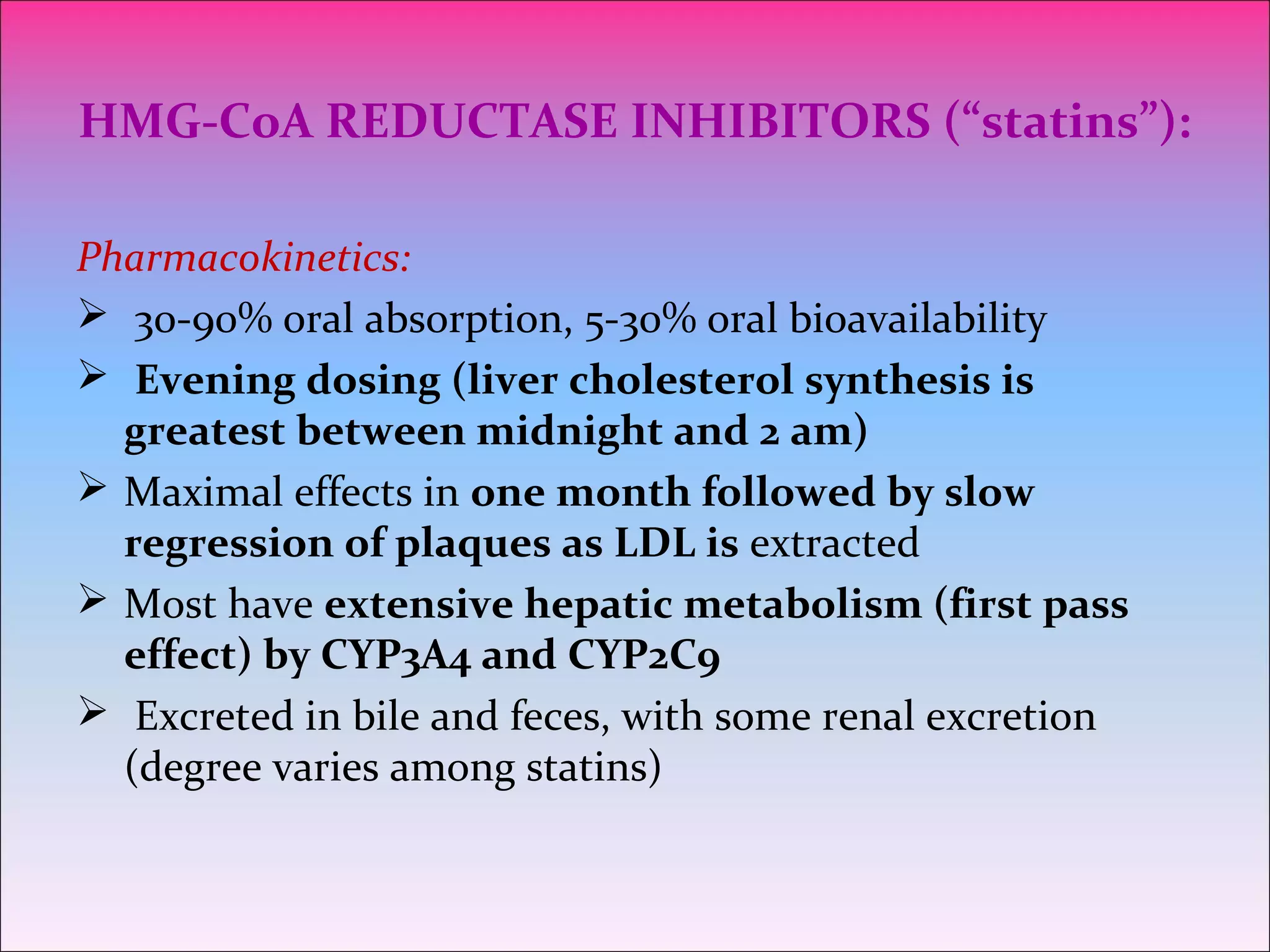
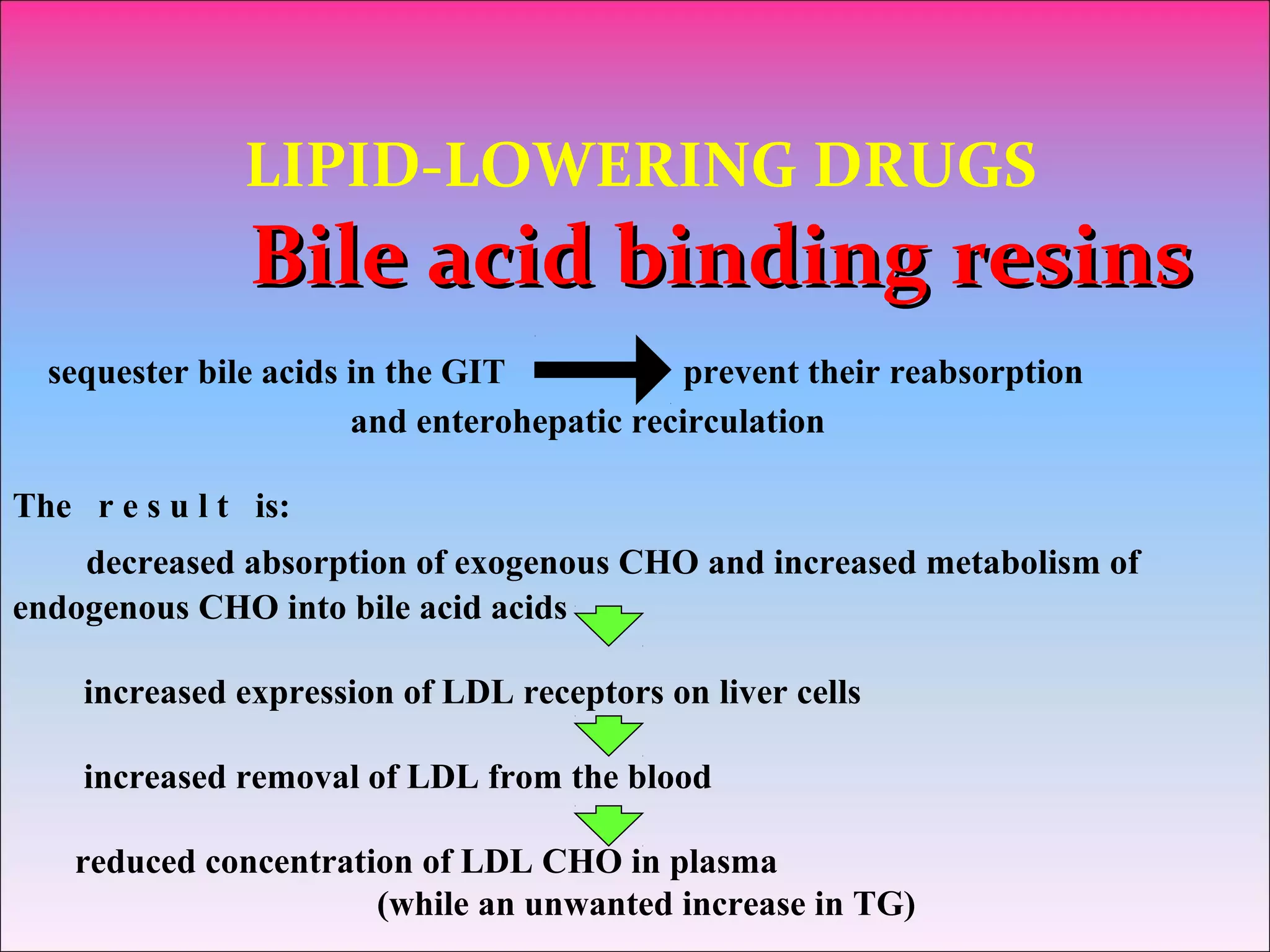
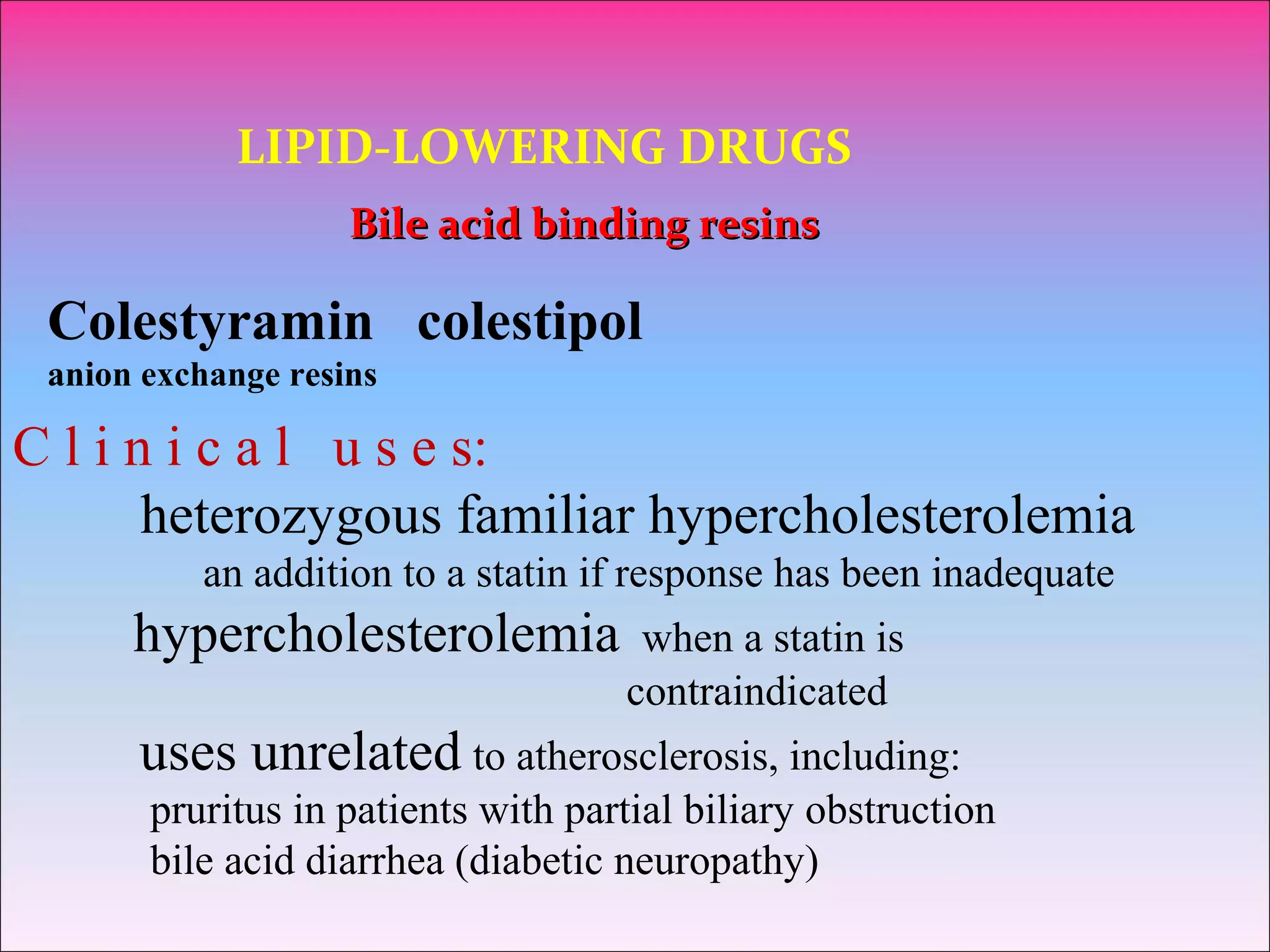
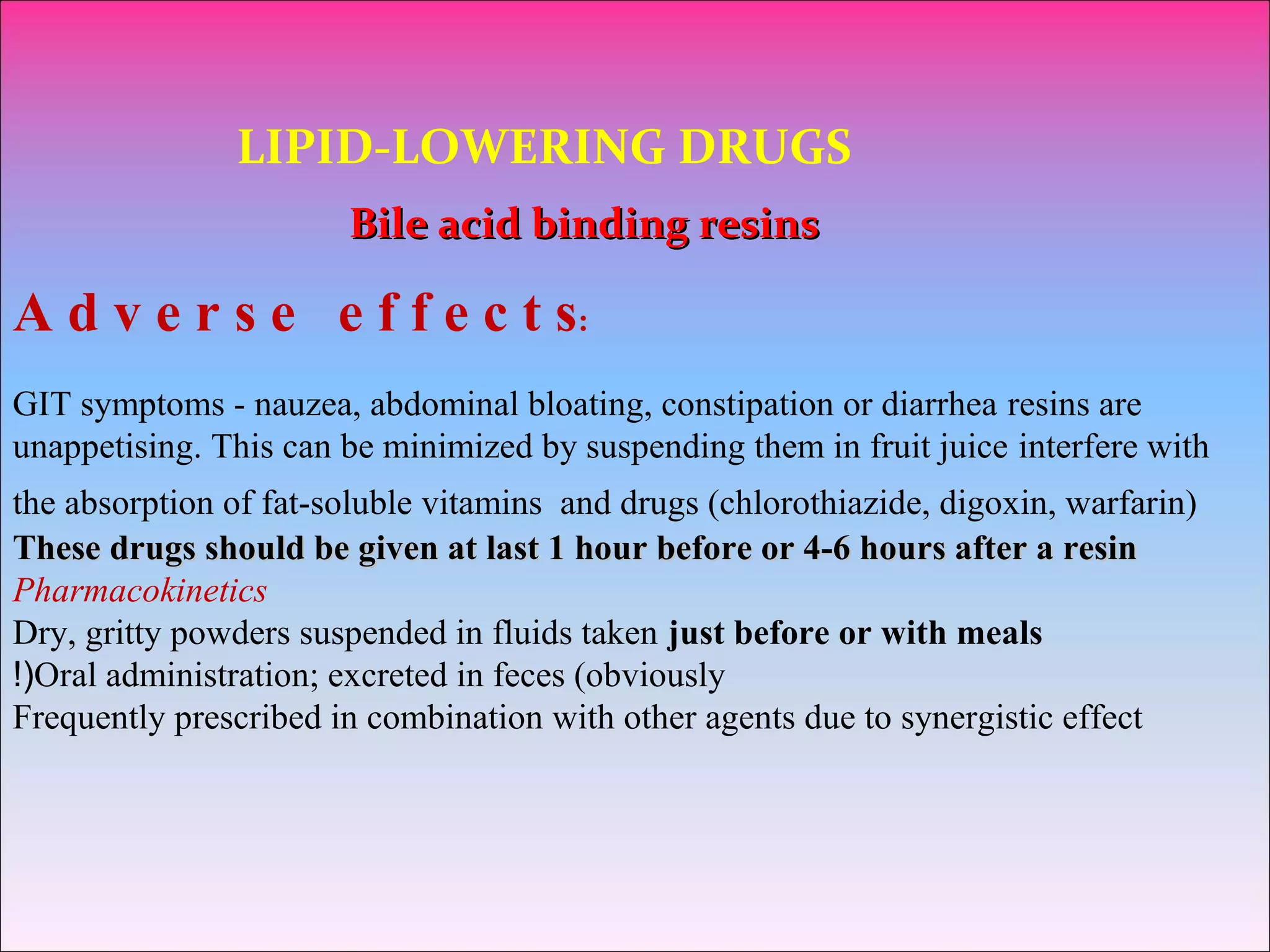
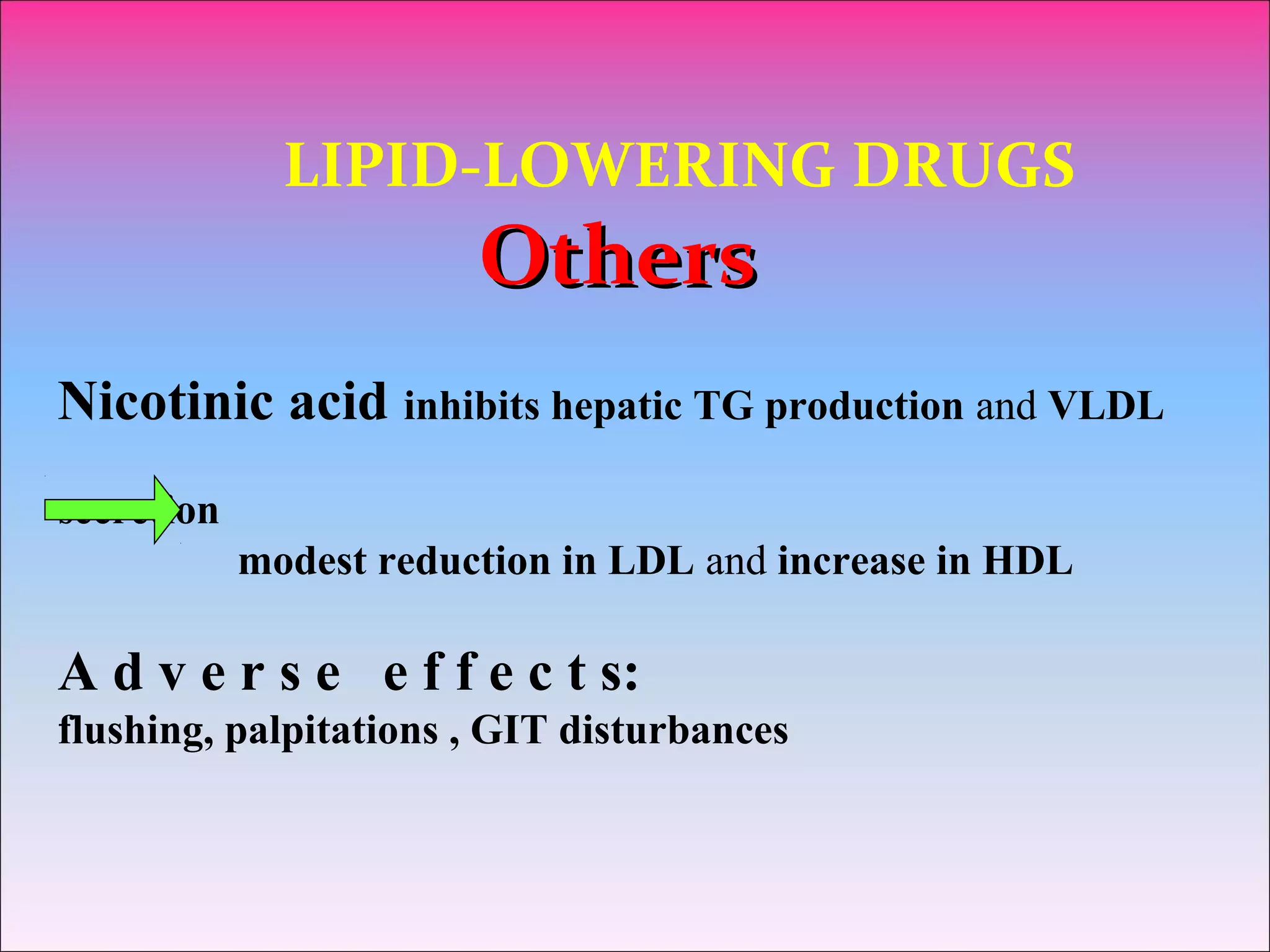
This document discusses lipid-lowering drugs used to treat hyperlipidemia and prevent cardiovascular disease. It covers the main classes of drugs including statins, fibrates, bile acid sequestrants, and niacin. Statins work by inhibiting cholesterol synthesis while fibrates activate lipoprotein lipase. Bile acid sequestrants bind bile acids in the gut. The document reviews the mechanisms, effects, uses, and side effects of these drug classes and emphasizes the importance of lifestyle modifications and managing hyperlipidemia.