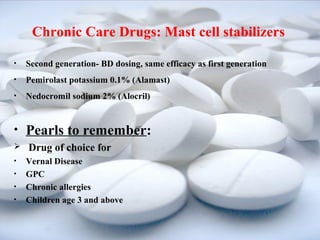
This document discusses various drug treatments for ocular allergies. It describes how allergic reactions cause the release of histamine and other inflammatory mediators from mast cells. The main classes of anti-allergy drugs discussed are ocular decongestants, antihistamines, mast cell stabilizers, NSAIDs, and corticosteroids. Specific examples of drugs in each class are provided along with their mechanisms of action and recommended dosages.