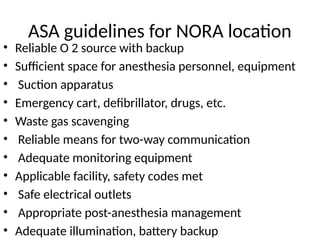
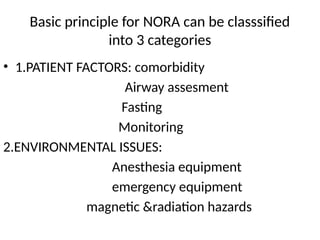
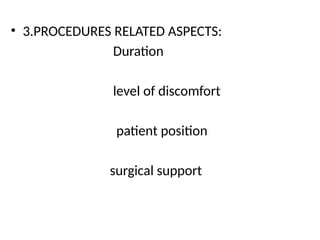
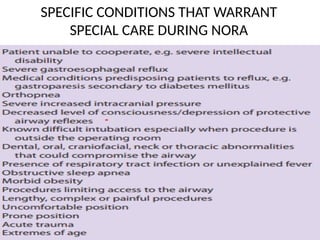
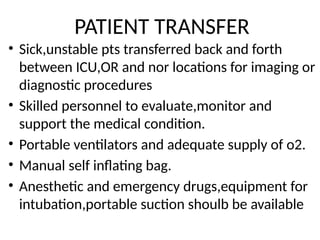
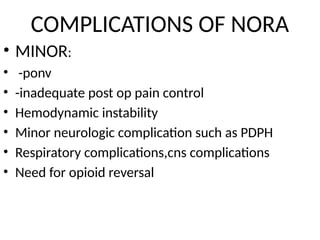
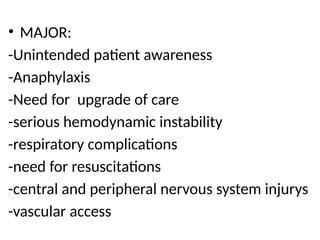
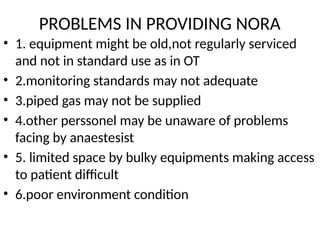
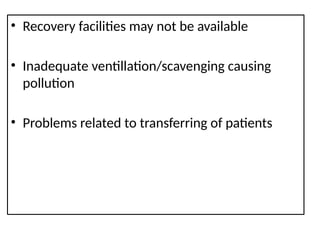
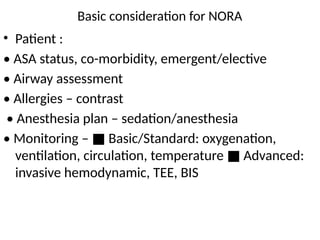
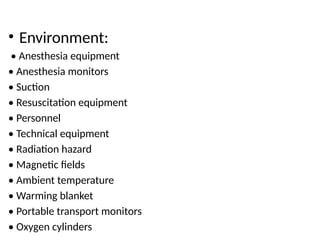
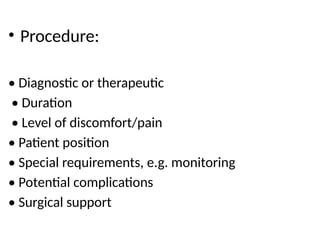
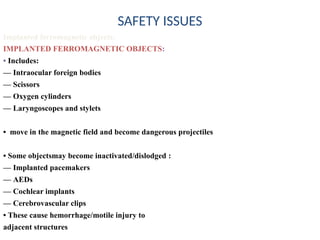
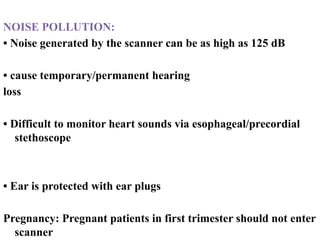
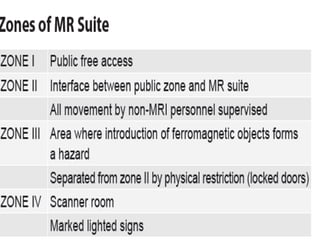
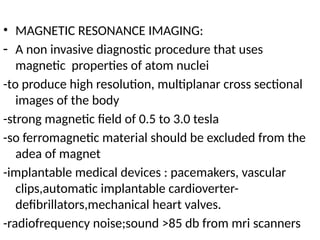
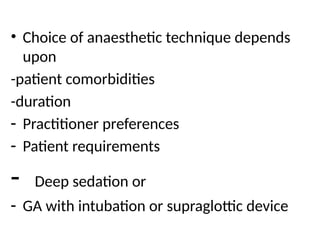
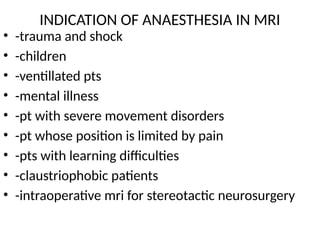
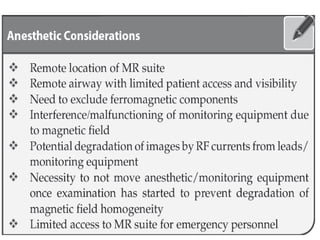
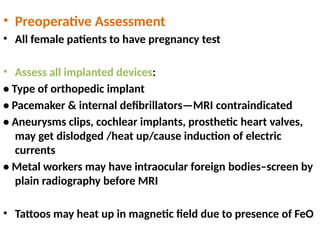
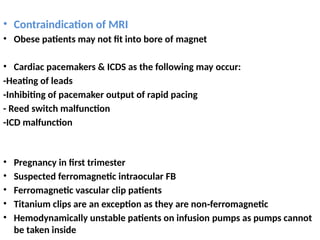
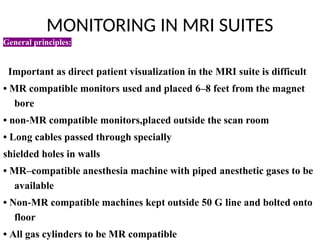
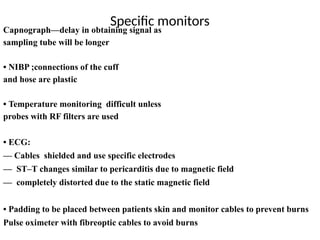
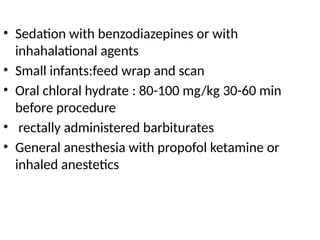
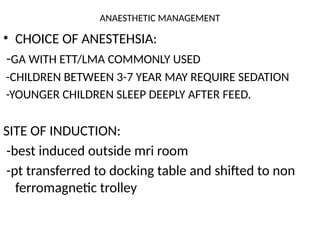
The document discusses non-operating room anesthesia (NORA), which includes procedures done outside of traditional operating rooms, highlighting the necessary guidelines such as equipment requirements and monitoring standards. It also addresses various environmental and operational challenges, potential complications, and specific considerations for different imaging and vascular intervention procedures. Key anesthetic management strategies for special populations, including children with hydrocephalus, are also covered, emphasizing the importance of preoperative assessments and customized approaches.