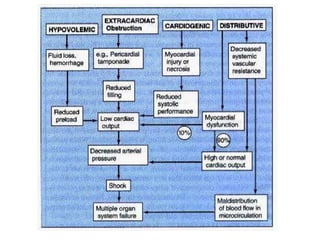
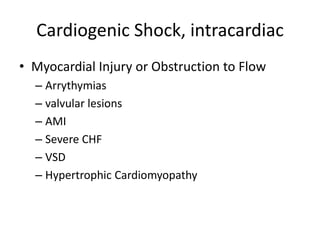
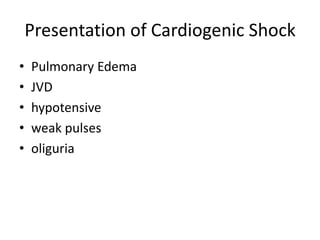
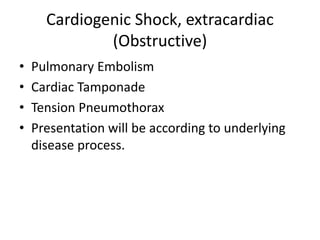
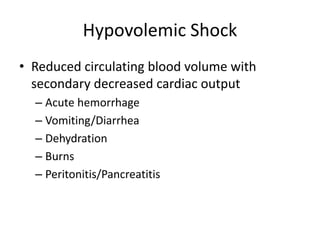
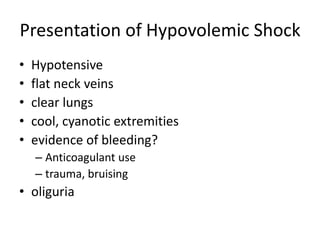
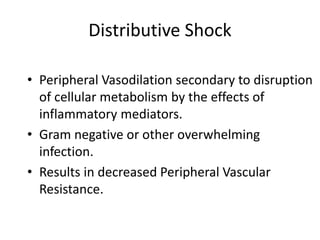
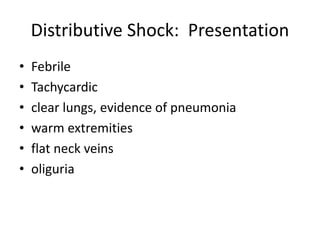
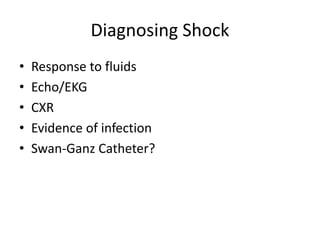
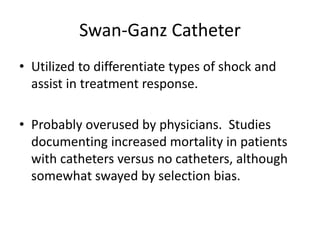
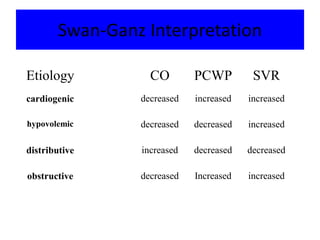
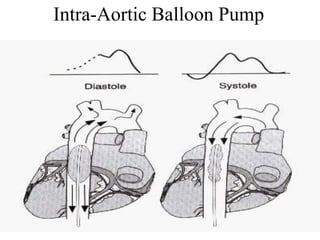
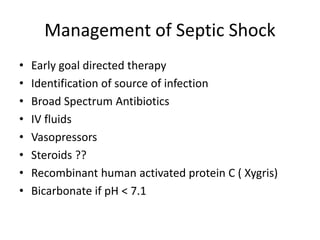
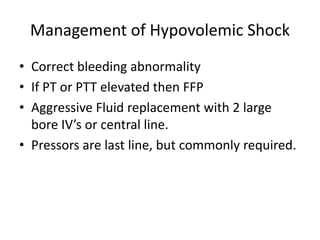
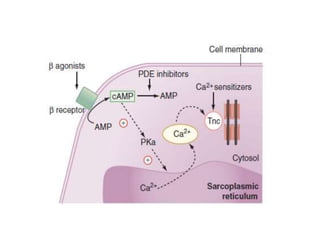
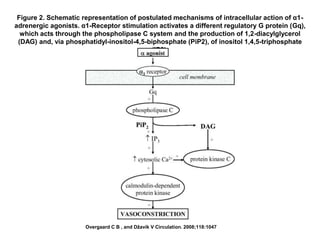
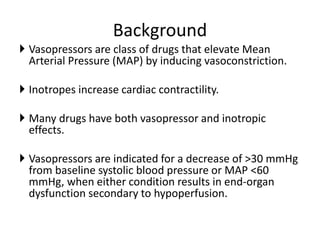
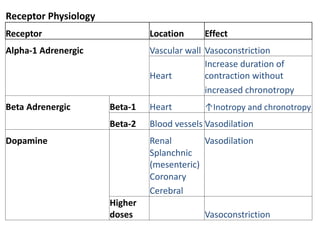
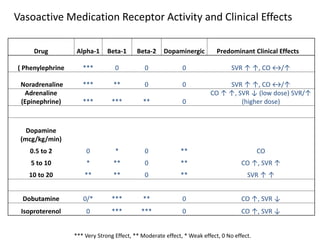
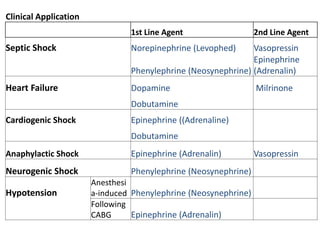
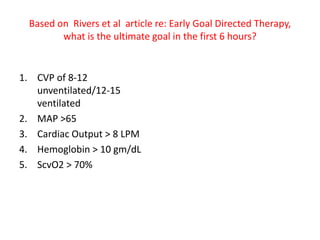
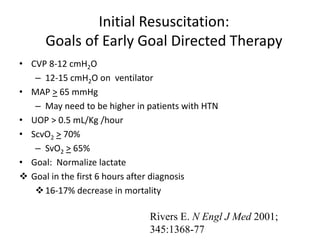
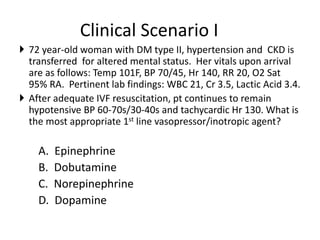
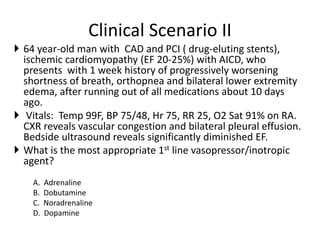
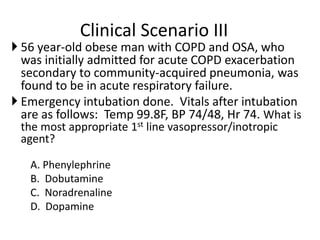
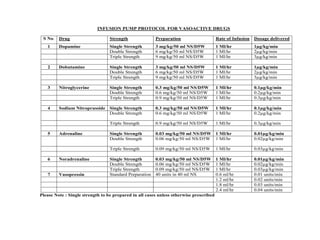
The document provides a comprehensive overview of different types of shock including cardiogenic, hypovolemic, and distributive shock, detailing their causes, presentations, and diagnostic approaches. It emphasizes the use of vasopressors and inotropes for managing blood pressure and cardiac output, alongside fluid resuscitation strategies tailored to the specific type of shock. Management protocols are outlined, including the early goal-directed therapy approach and specific clinical scenarios for vasopressor selection.