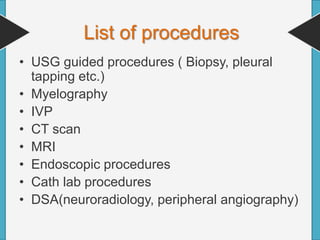
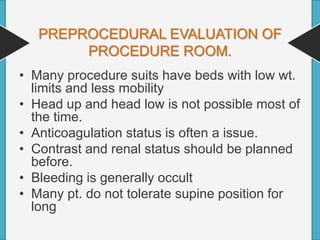
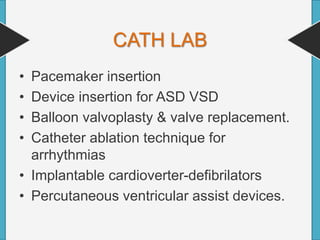
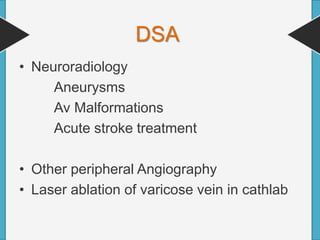
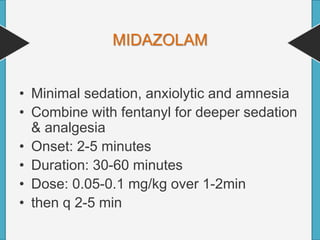
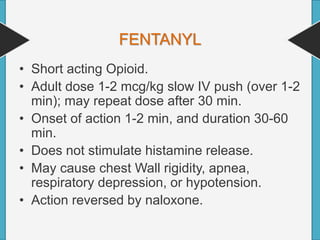
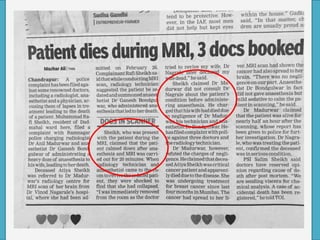
This document discusses the unique constraints anesthesiologists face when providing care in radiology settings rather than traditional operating rooms. It notes that radiological procedures generate significant volume and revenue, and require the same attention to efficiency, planning, and consistency as major surgeries. The document outlines general constraints like equipment limitations, monitoring challenges, and communication barriers in radiology suites. It also provides anesthesia considerations and approaches for specific radiological procedures like CT, MRI, cath lab cases, and interventional radiology.