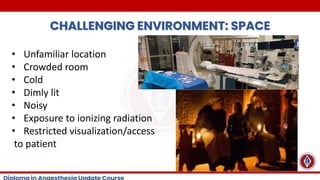
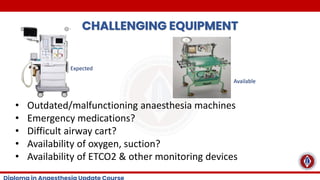
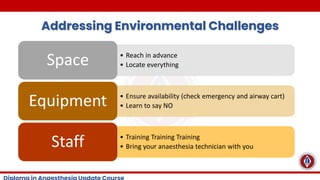
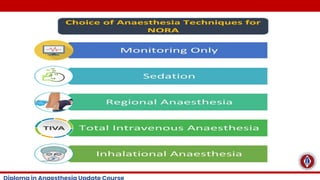
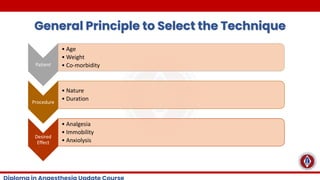
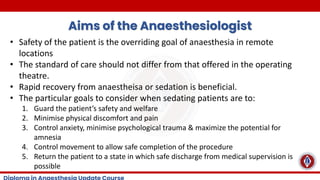
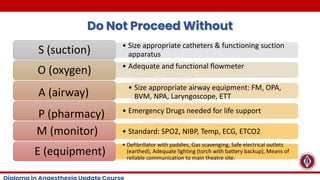
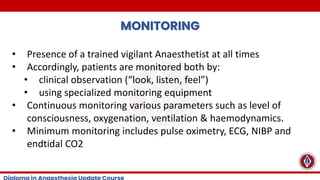
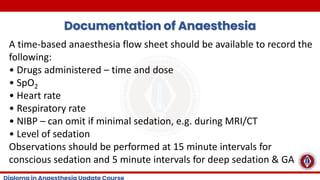
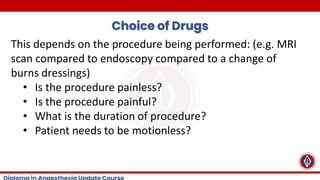
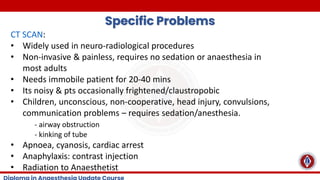
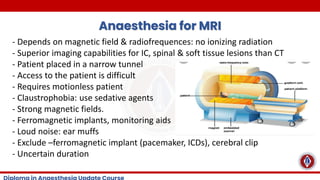
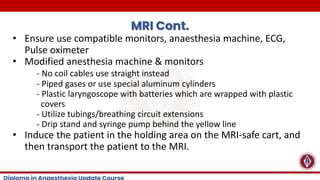
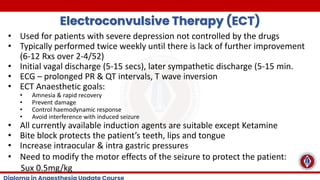
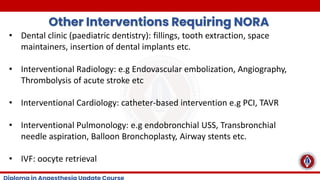
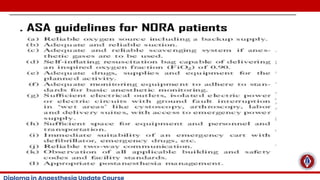
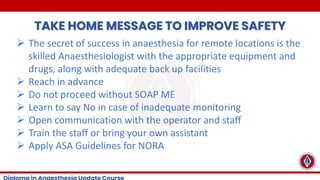
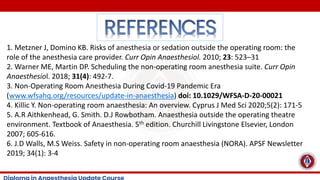
This lecture covers Anaesthetic considerations for Anaesthesia outside the operating room, remote areas and also interventional suites. This also covers preparation for such Anaesthetia and anticipating possibile complications with on the ground plan to mitigate such complications.