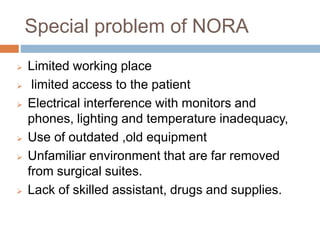
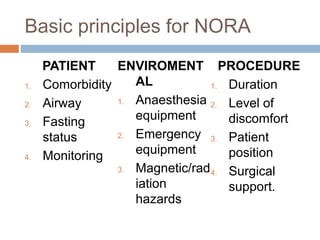
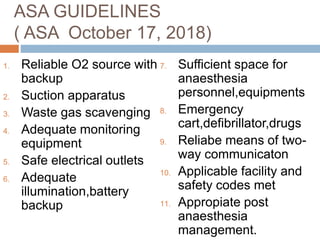
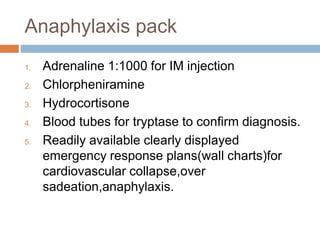
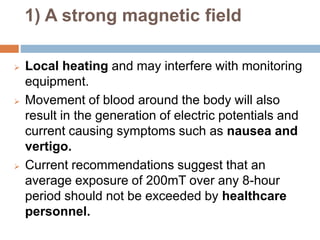
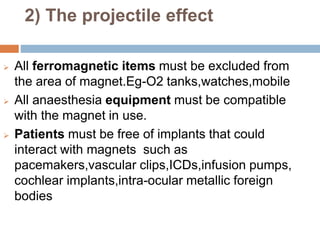
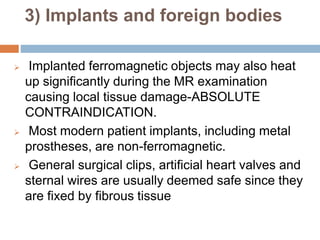
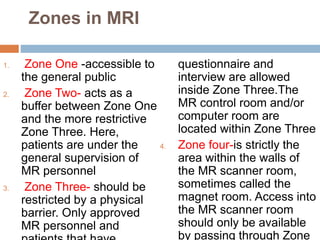
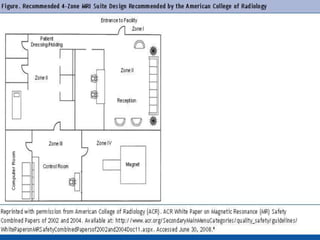
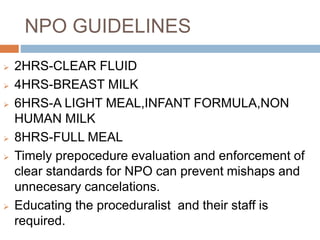
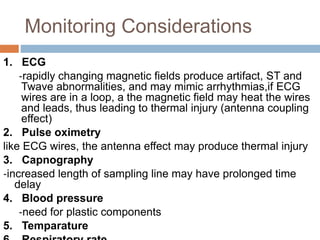
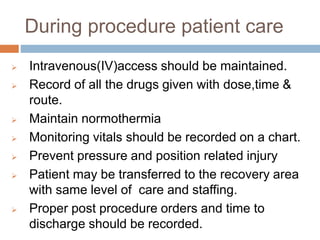
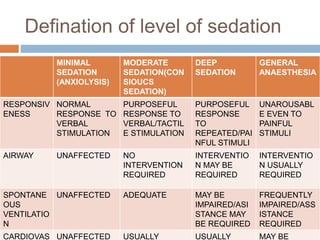
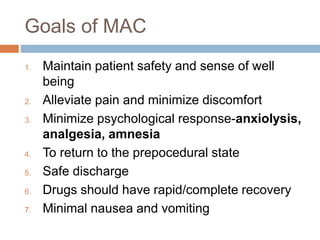
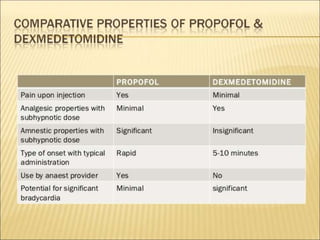
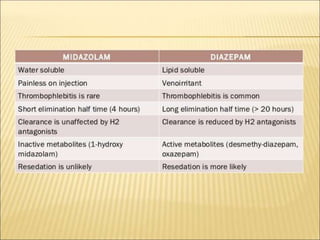
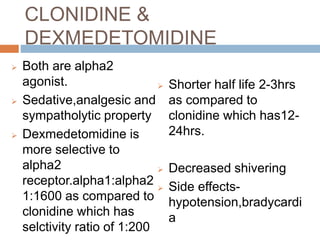
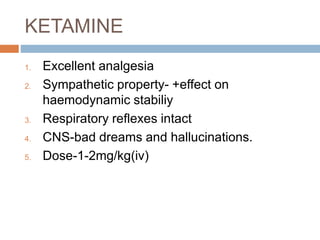
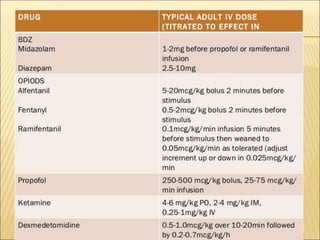
This document discusses guidelines and considerations for providing anaesthesia services in non-operating room areas (NORA) such as for MRI/CT scans. It notes special challenges in NORA including limited space, equipment issues, and unfamiliar environments. Key guidelines are outlined such as having proper patient monitoring, emergency equipment, and following pre-procedure evaluations. Specific anaesthetic drugs that can be used for moderate sedation are discussed, including propofol, benzodiazepines, dexmedetomidine, and ketamine. Hazards in the MRI environment like magnetic fields, acoustic noise, and restricted access are summarized. The document stresses the importance of patient safety, standards of care, and proper planning for NORA cases.