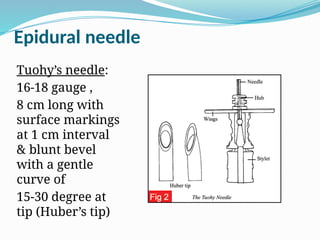
The document discusses the anatomy, advantages, disadvantages, indications, contraindications, and techniques for epidural anaesthesia. Key points include the structure and contents of the epidural space, the types of local anaesthetics used, and the importance of careful administration to avoid complications. It also compares epidural and spinal blocks, emphasizing their differences in dosage, technique, and safety concerns.