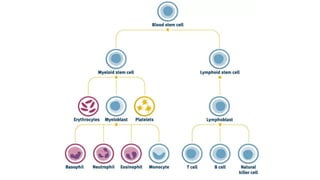
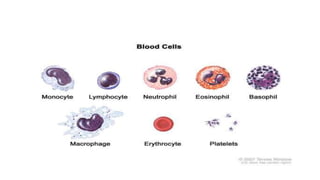
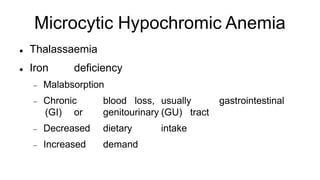
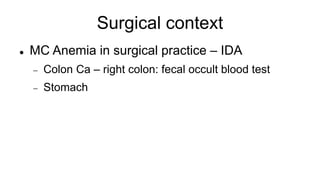
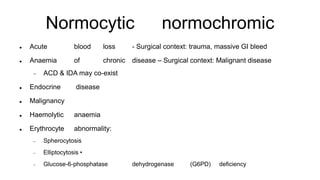
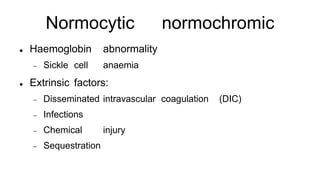
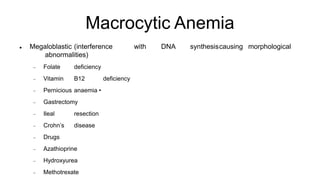
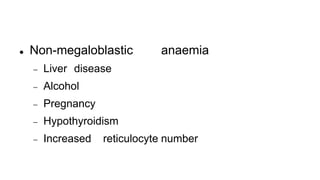
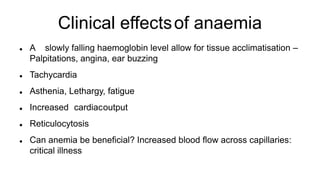
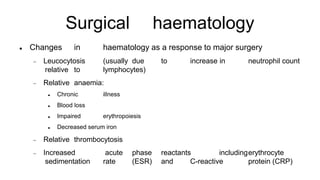
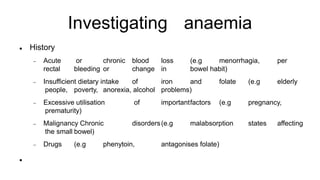
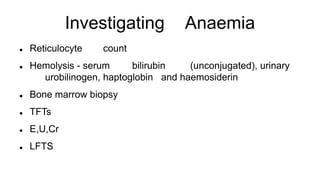
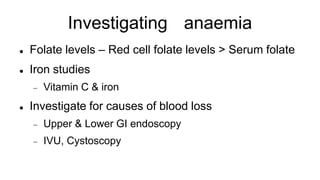
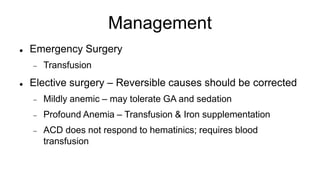
This document discusses anemia in the context of surgery. It begins by defining anemia and describing the composition of blood. It then classifies anemias by size, color, and cause, including microcytic hypochromic anemias such as iron deficiency anemia, normocytic normochromic anemias caused by blood loss or disease, and macrocytic anemias such as megaloblastic or non-megaloblastic types. Clinical effects of anemia and hematologic changes after surgery are reviewed. The document outlines how to investigate the cause of anemia and manage anemia in surgical patients, including blood transfusions, correcting reversible causes, and hematinic supplementation.