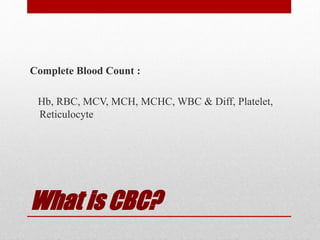
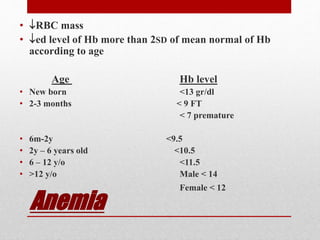
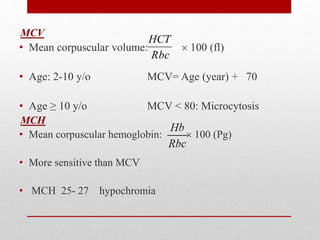
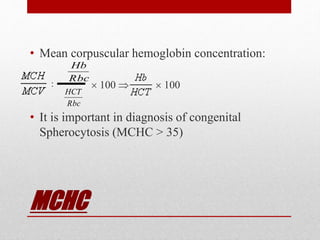
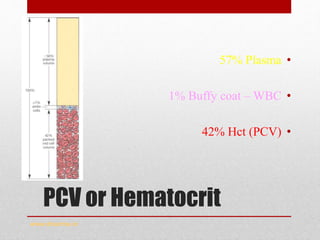
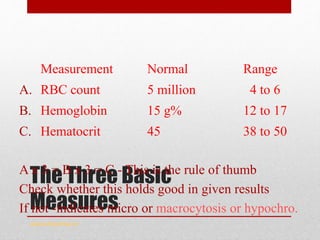
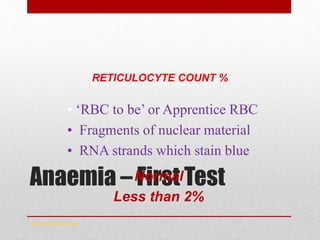
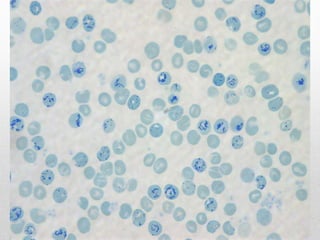
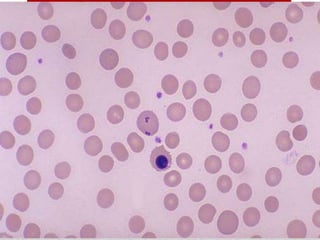
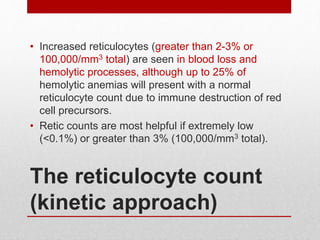
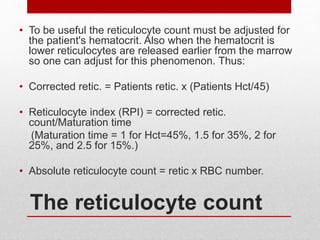
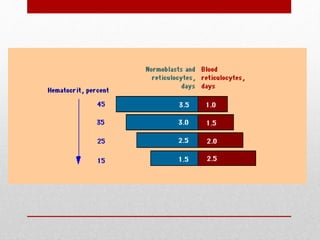
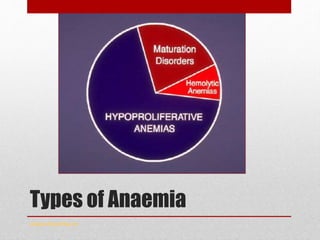
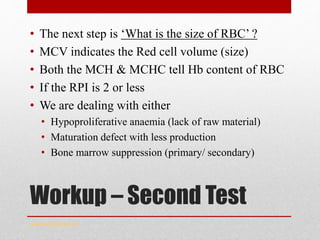
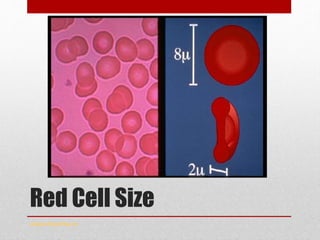
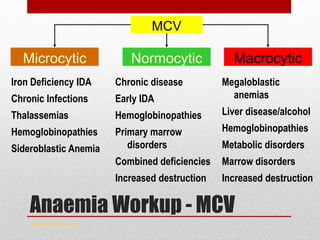
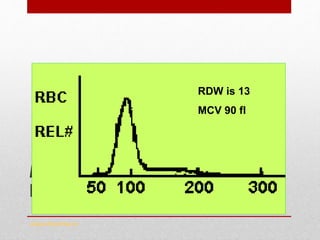
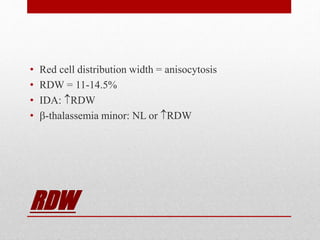
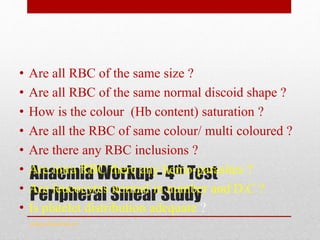
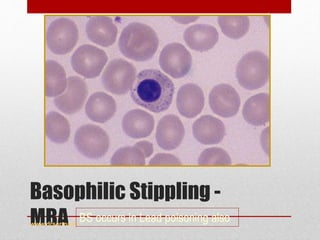
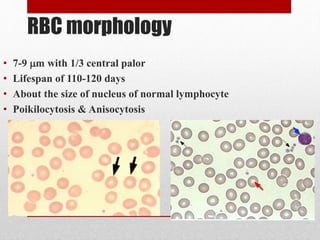
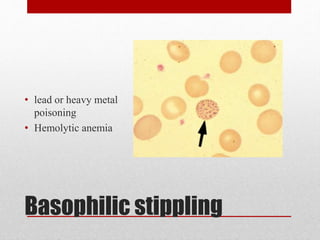
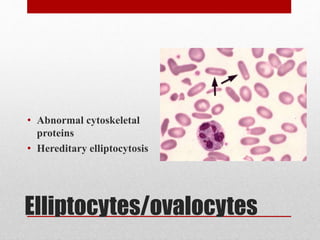
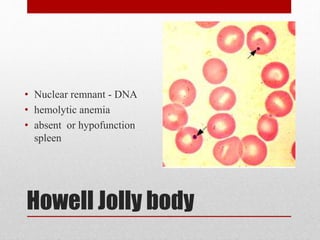
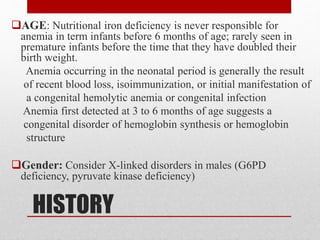
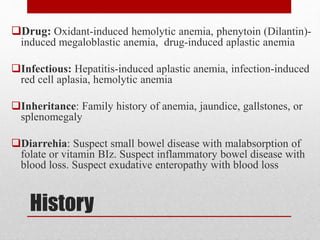
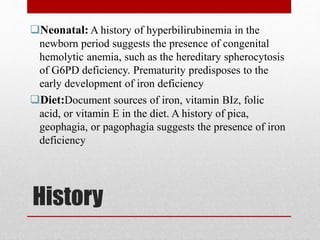
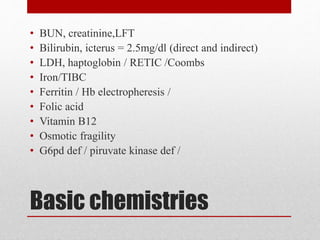
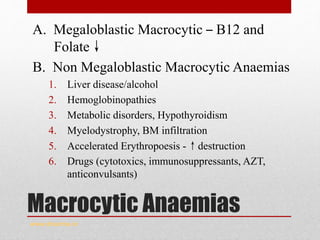
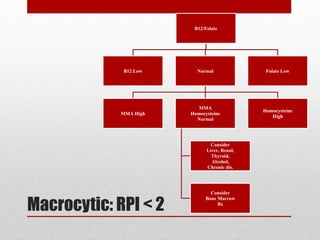
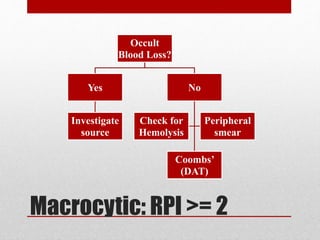
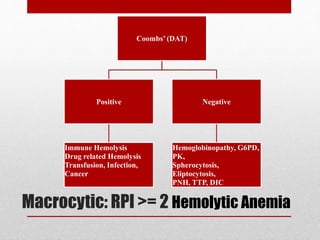
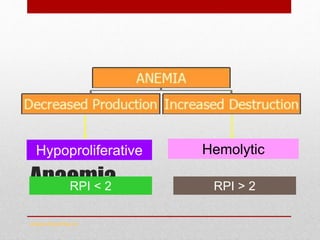
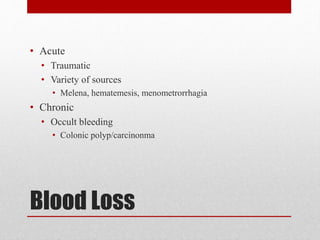
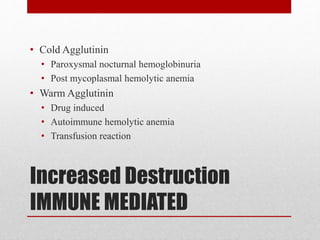
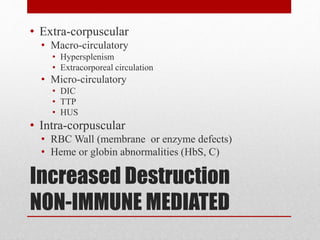
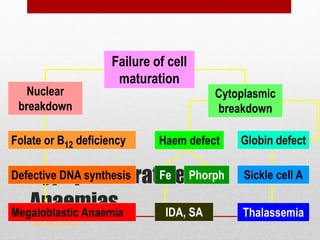
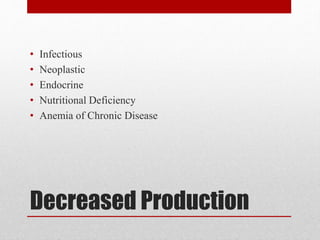
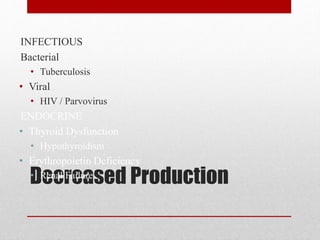
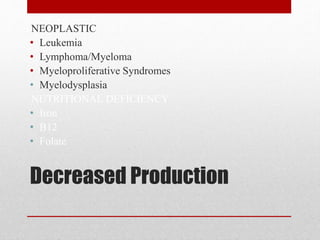
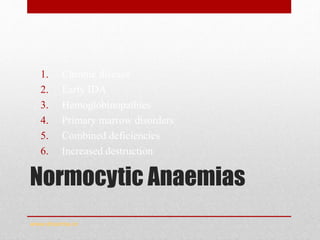
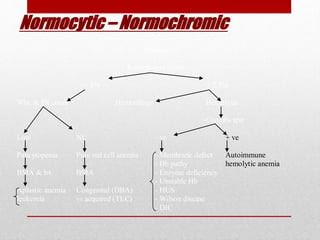
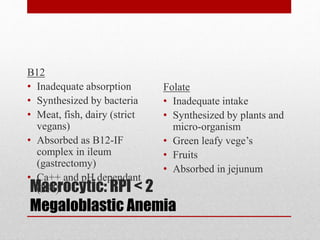
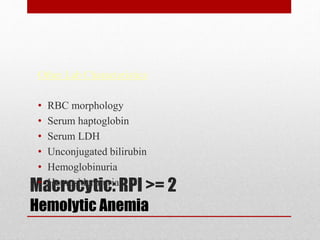
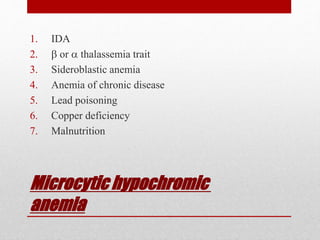
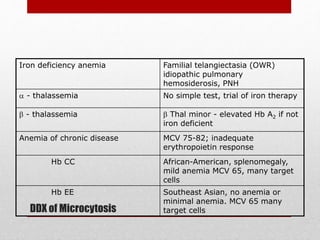
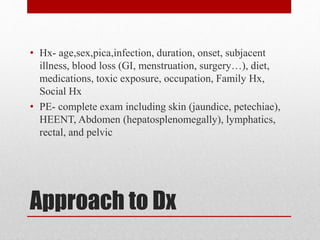
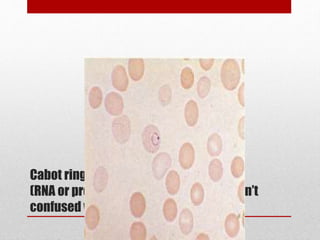
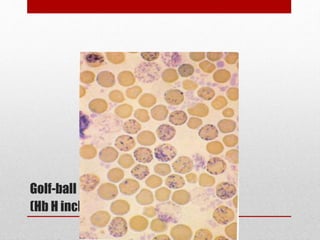
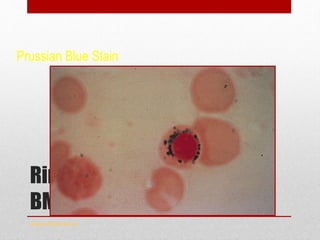
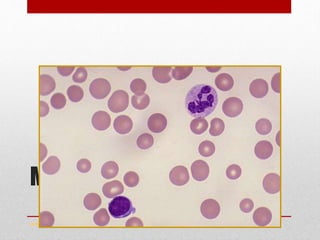
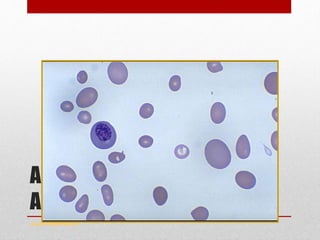
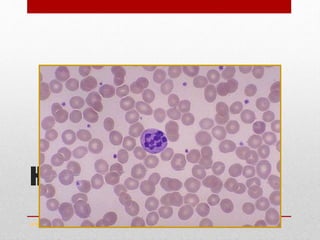
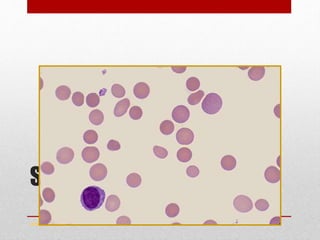
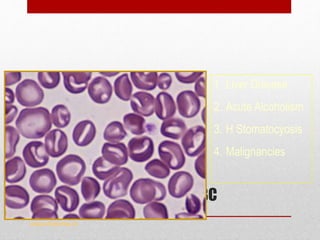
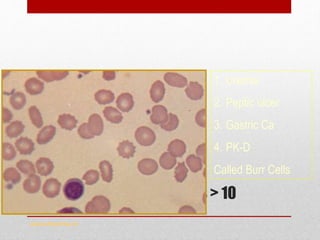
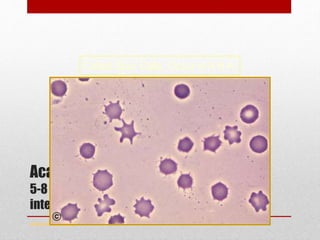
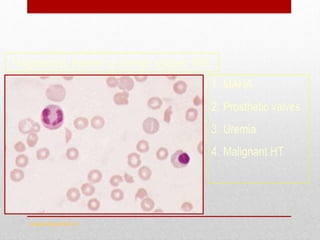
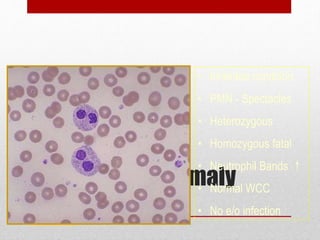
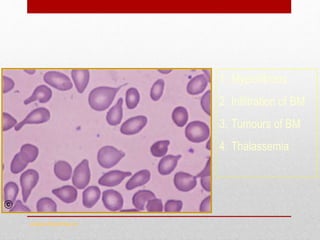
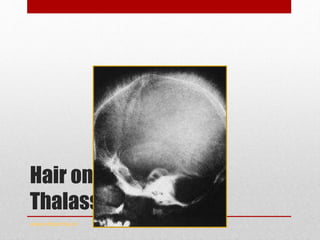
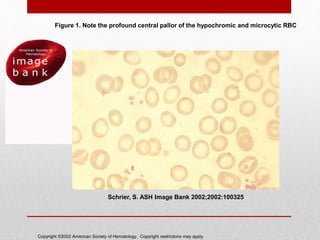
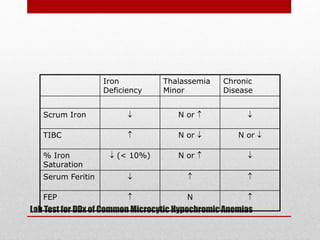
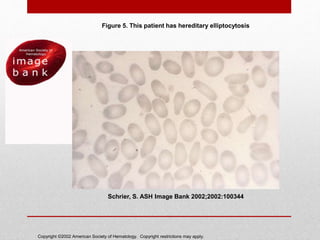
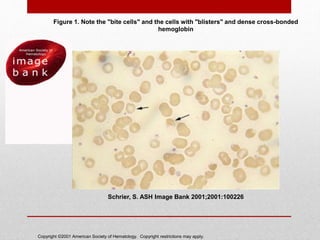
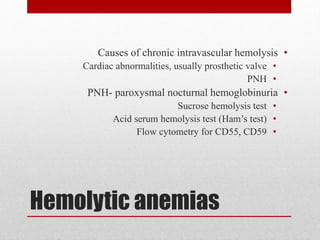
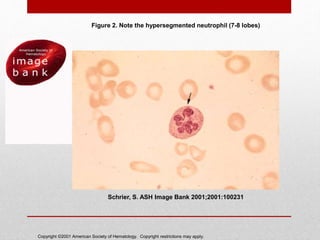
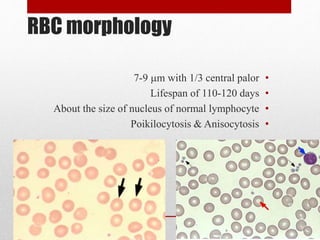
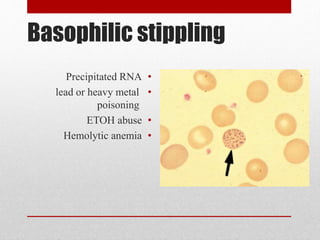
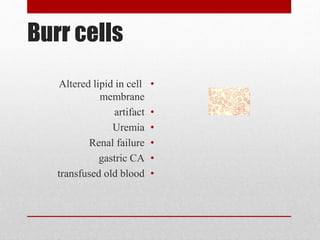
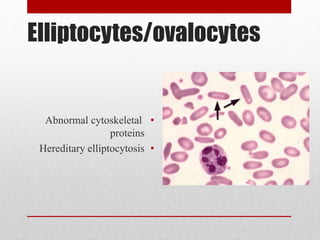
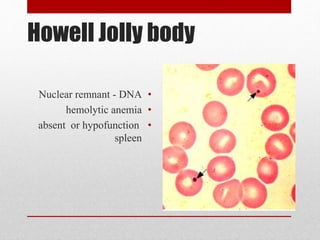
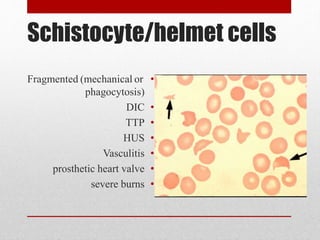
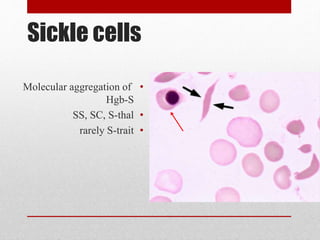
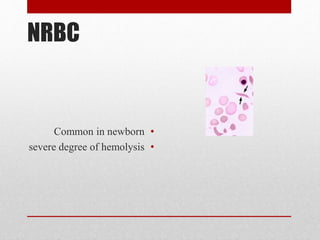
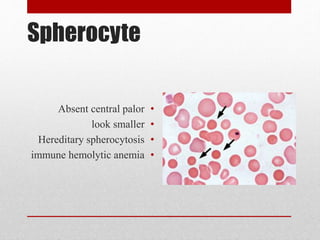
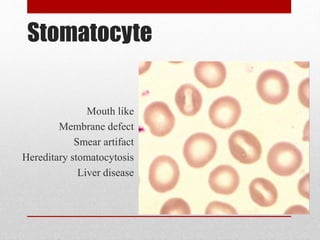
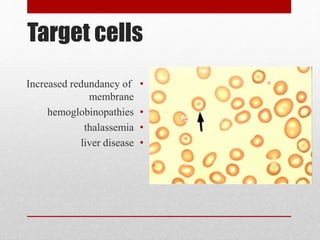
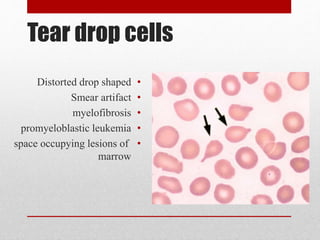
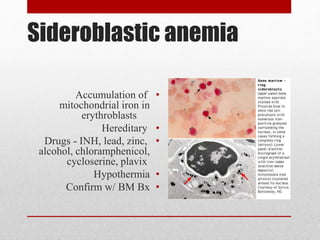
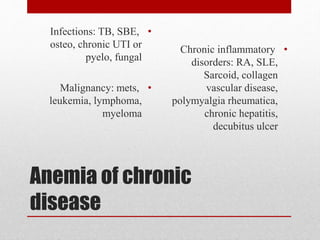
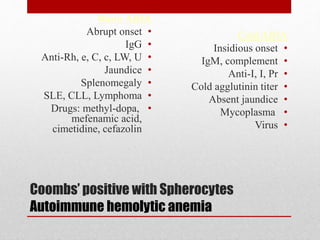
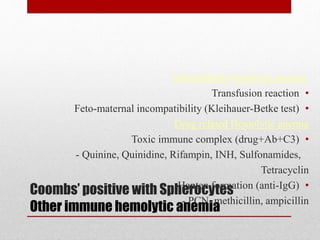
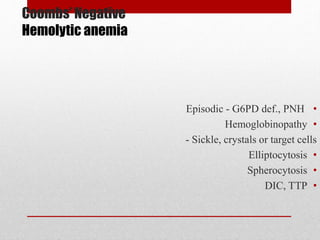
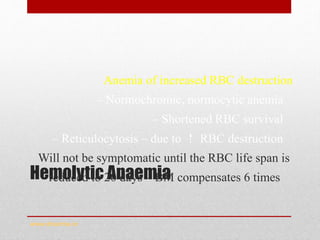
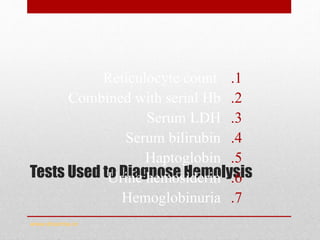
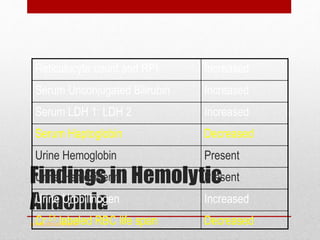
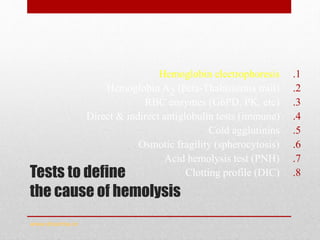
This document provides an overview of how to approach and evaluate anemia. It begins by defining anemia and describing a complete blood count. It then discusses evaluating the size, hemoglobin content, and distribution of red blood cells to classify anemia as microcytic, normocytic, or macrocytic. For each type of anemia, the document lists potential causes and recommends further tests. It also covers evaluating reticulocyte count, peripheral smear, and bone marrow biopsy findings to determine if anemia is caused by blood loss, increased destruction, or decreased production of red blood cells. The goal is to systematically narrow down the cause of anemia through a series of blood tests and examinations.