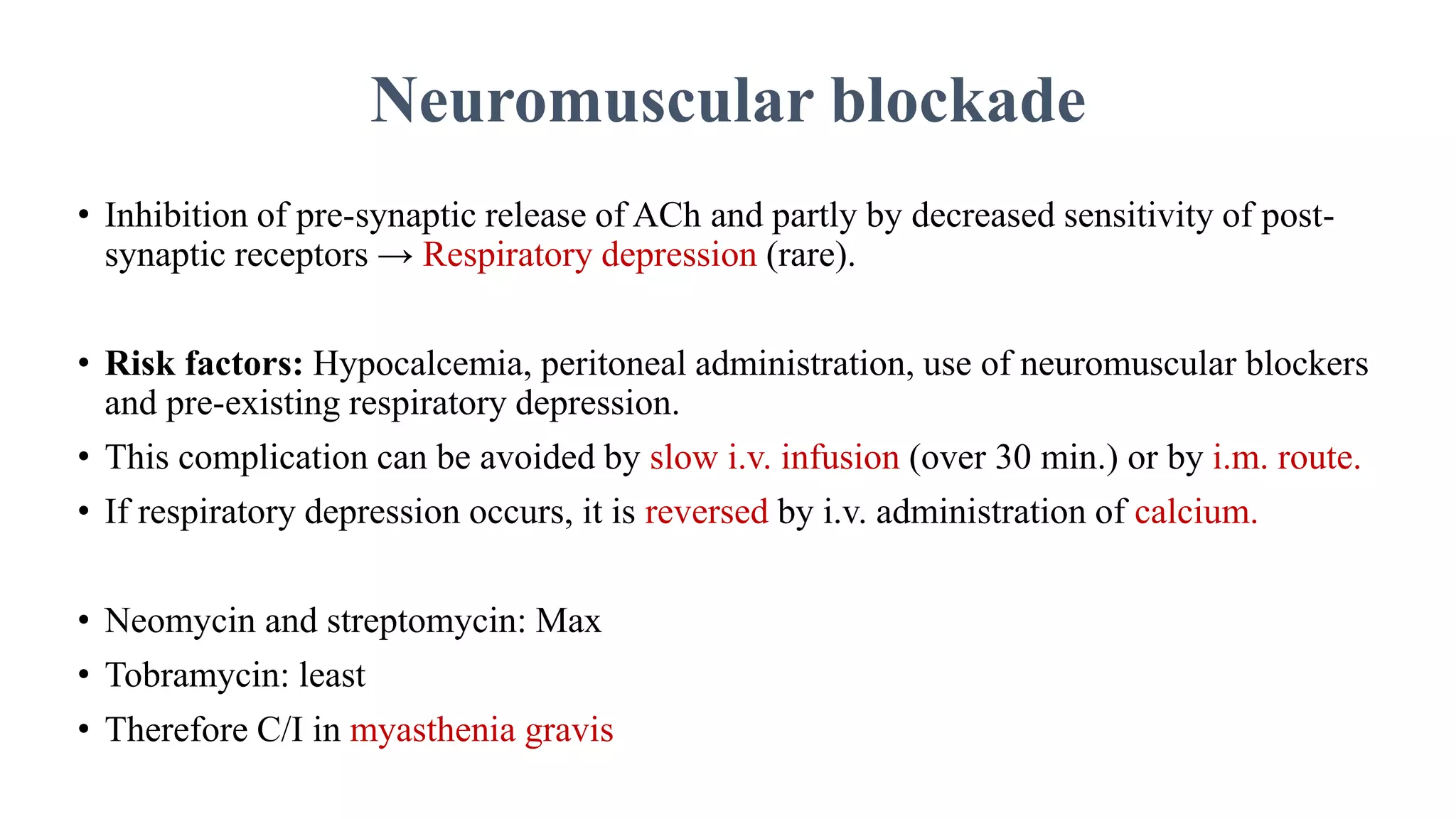
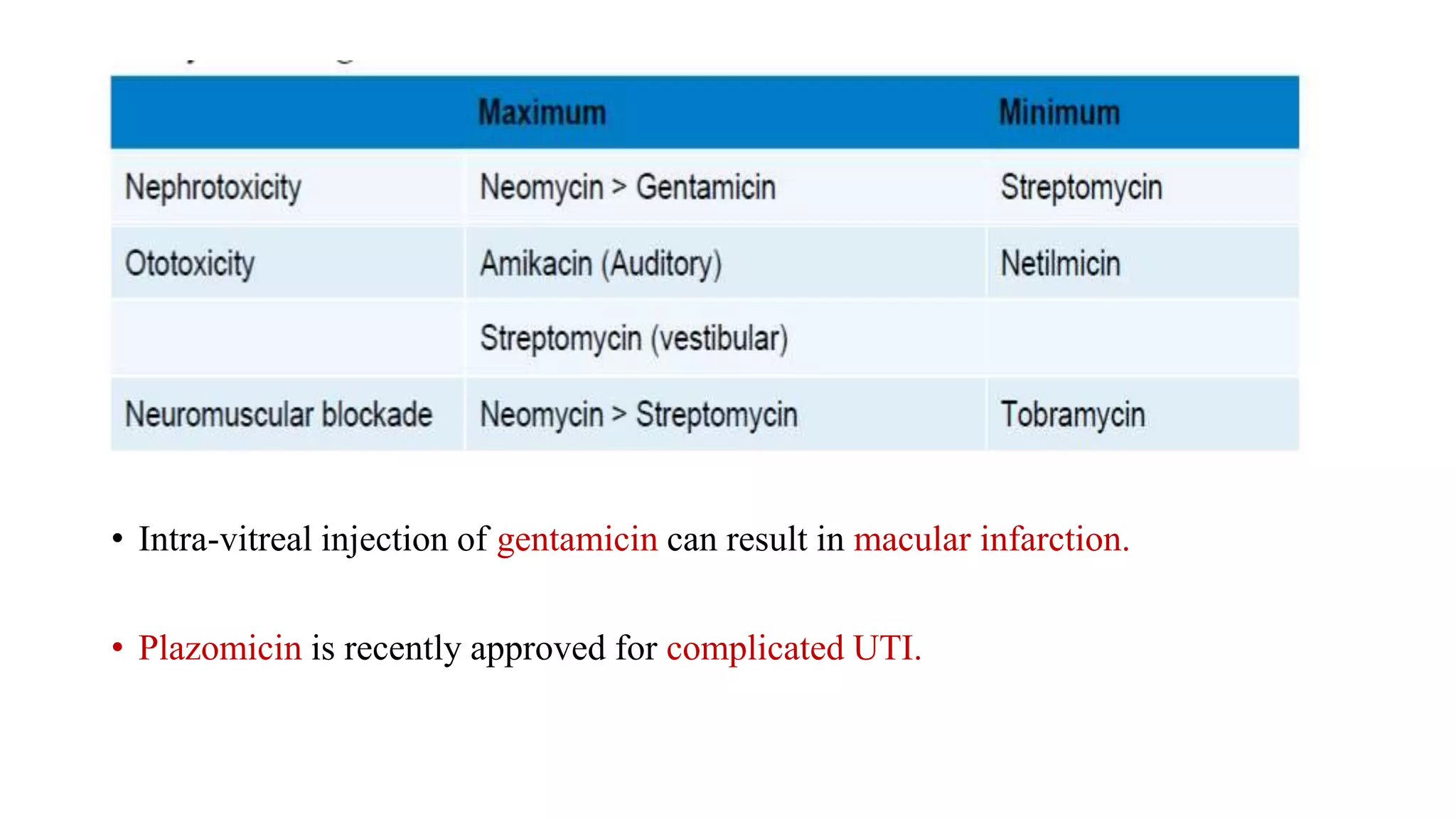
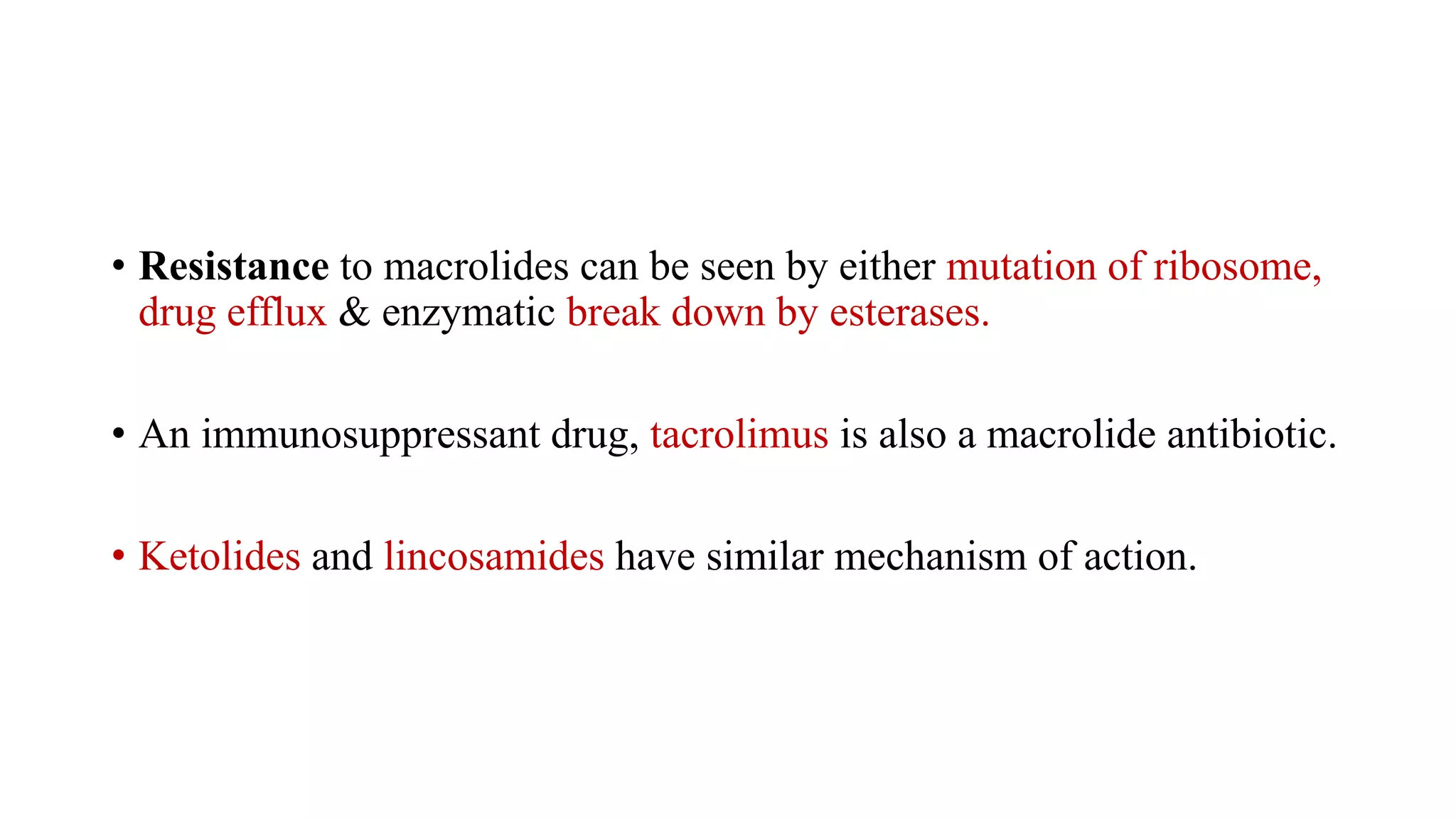
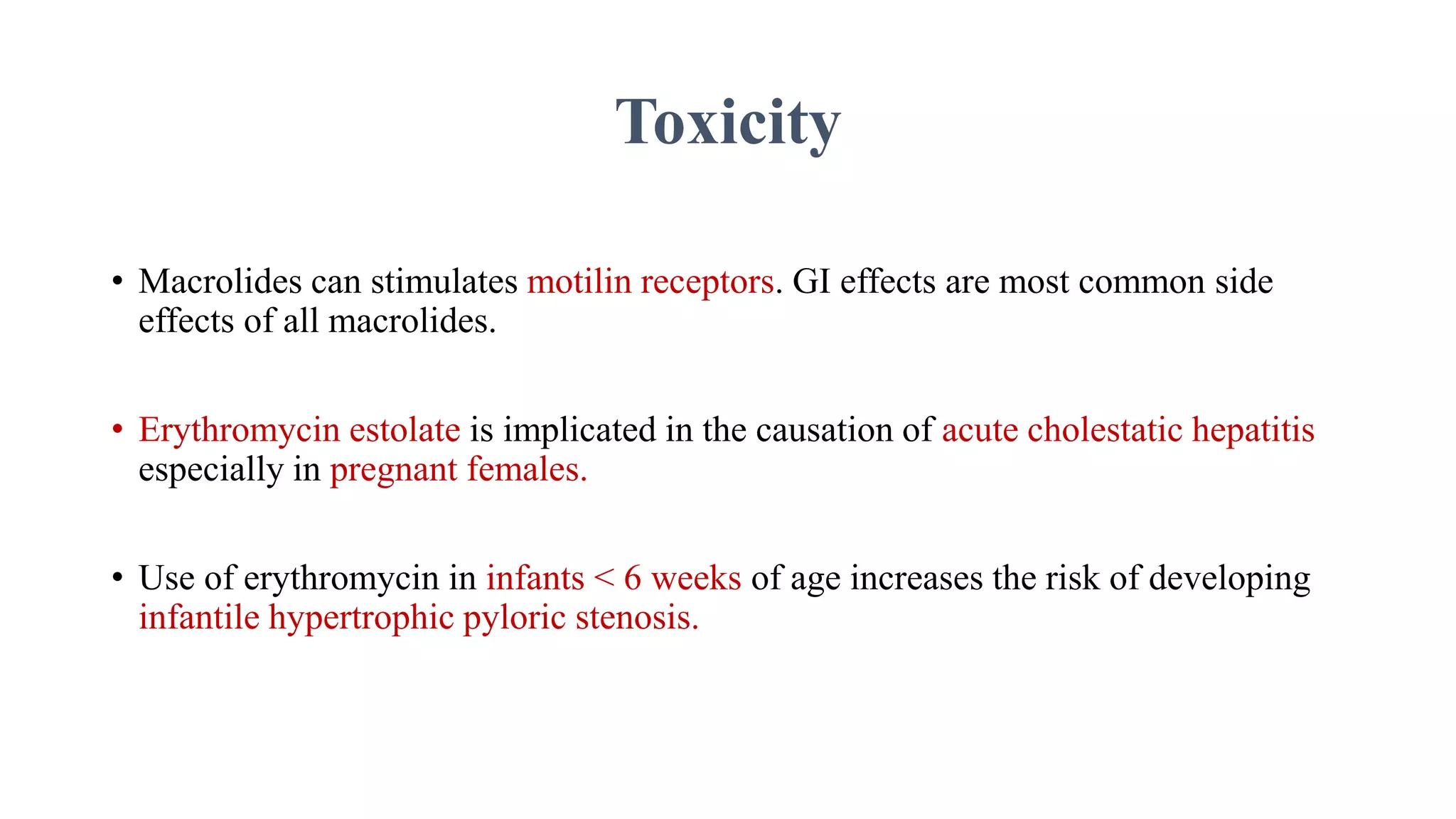
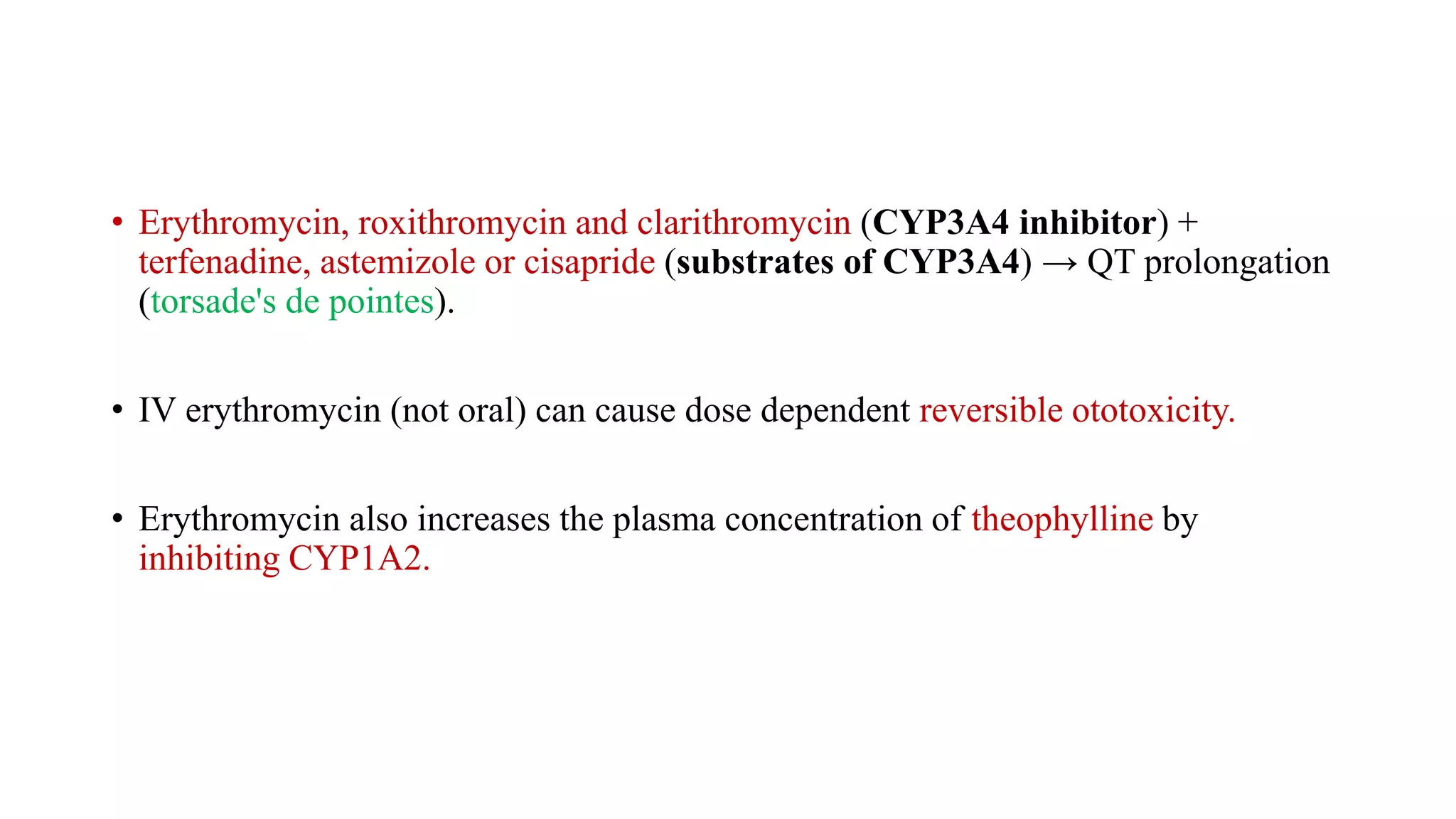
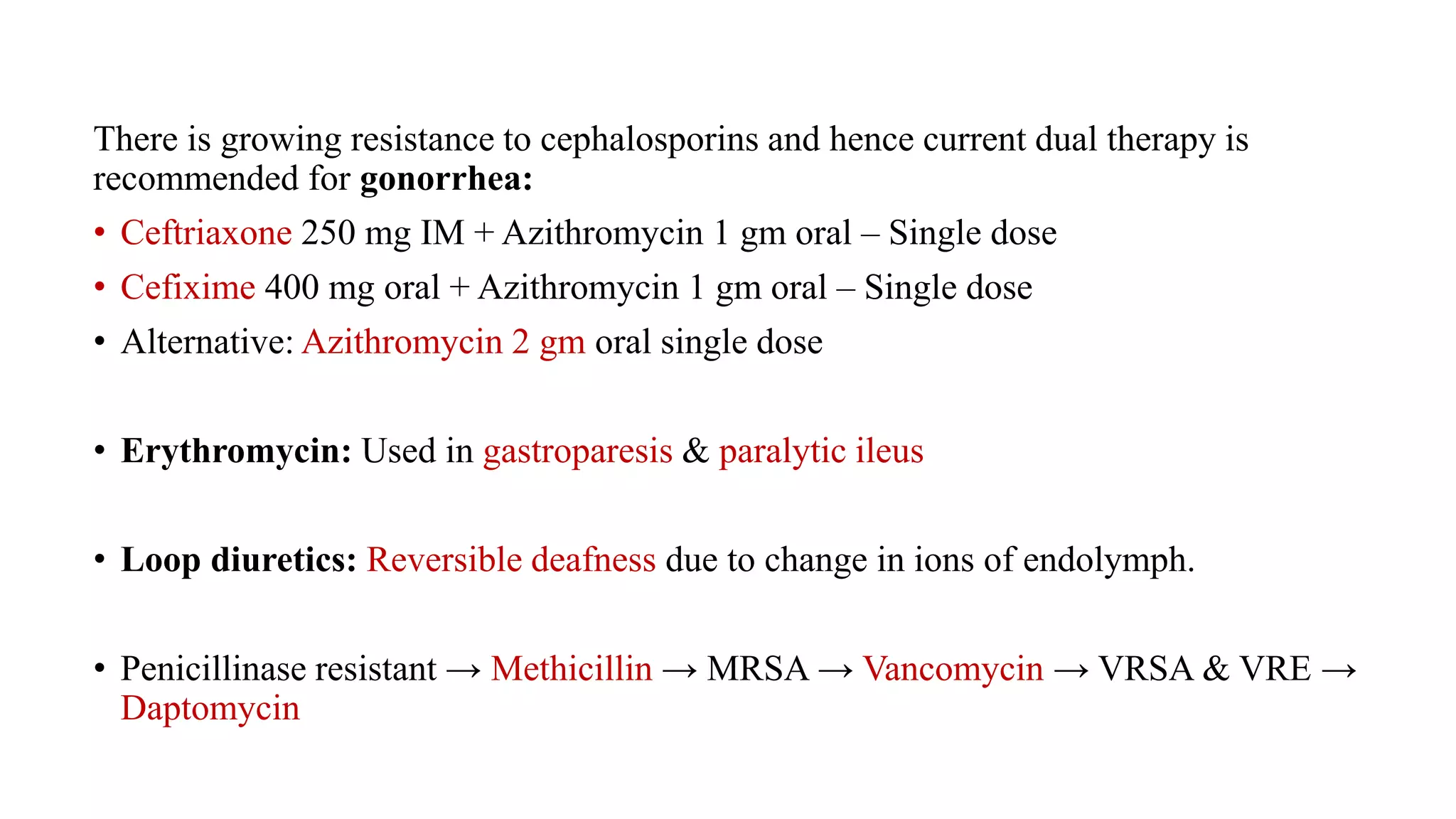
The document provides a comprehensive overview of aminoglycosides and macrolides, detailing their mechanism of action, clinical uses, pharmacokinetics, and potential toxicities. Aminoglycosides are bactericidal antibiotics effective primarily against gram-negative organisms, while macrolides are mainly bacteriostatic drugs effective against both gram-positive and certain atypical organisms. It also discusses precautions, drug interactions, and the growing issue of antibiotic resistance.