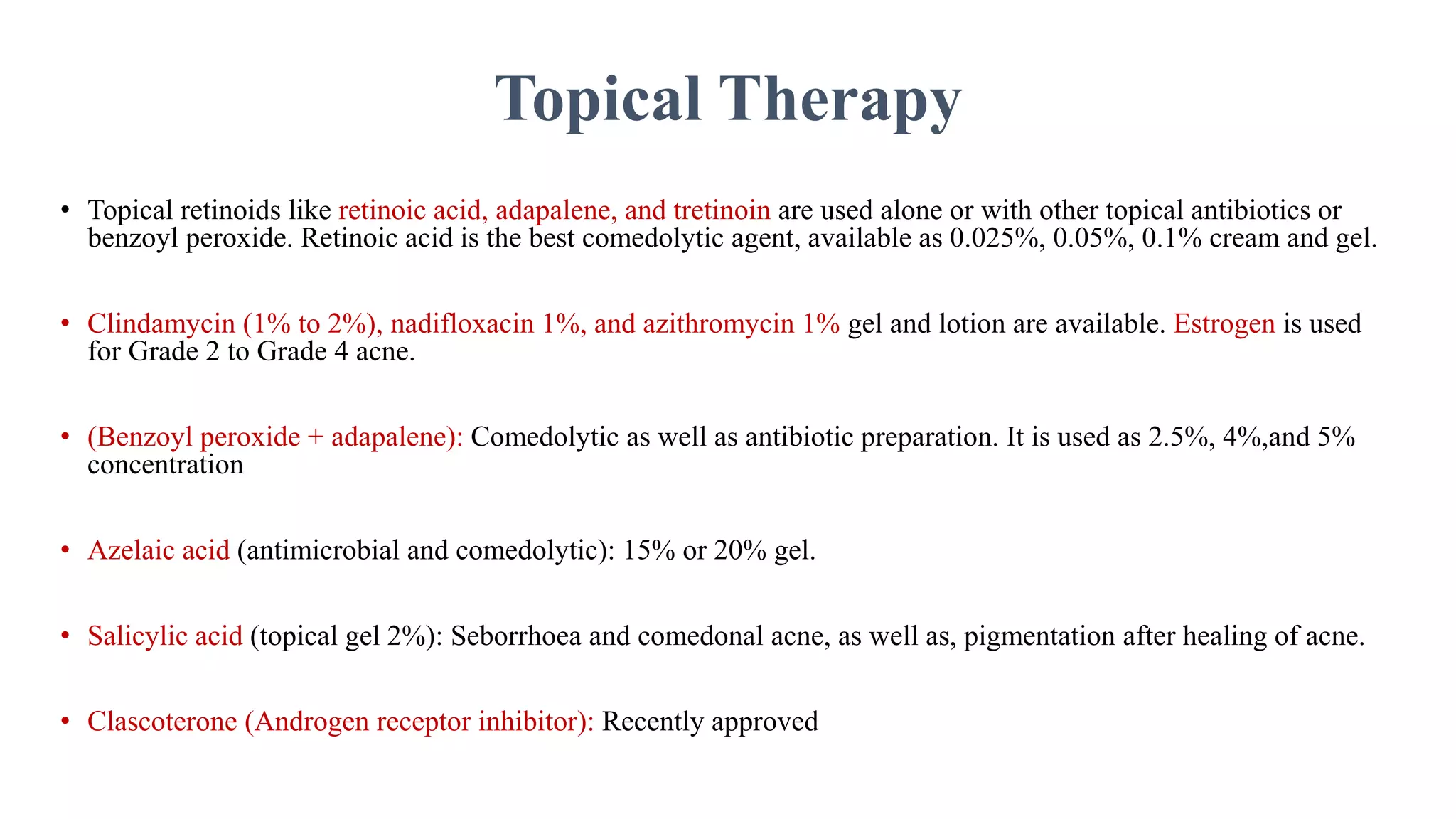
This document discusses recent advances in pharmacotherapy for various dermatological diseases. It covers treatment options for common conditions like vitiligo, acne, psoriasis, and androgenetic alopecia. For these conditions, it describes both topical and systemic drug therapy options, including corticosteroids, retinoids, antibiotics, isotretinoin, JAK inhibitors, and phototherapy. It also provides details on specific drugs, dosages, and mechanisms of action for treating various dermatological diseases.