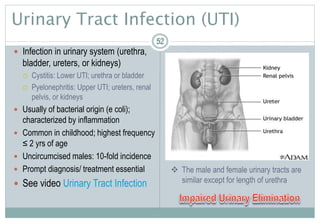
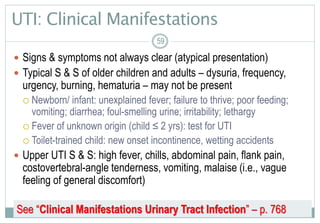
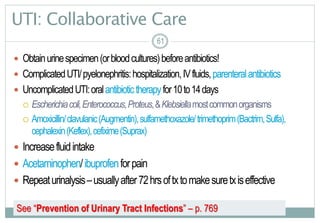
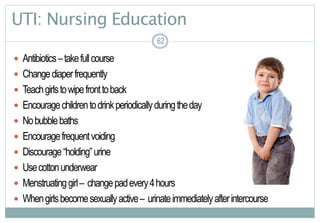
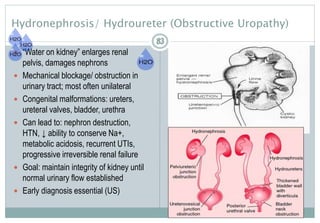
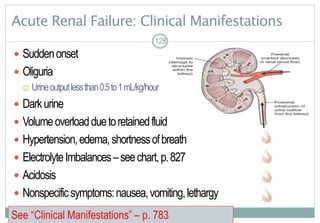
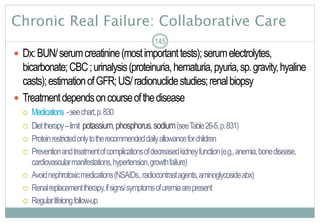
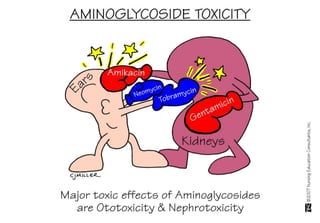
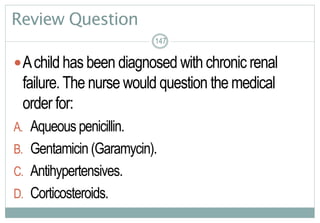
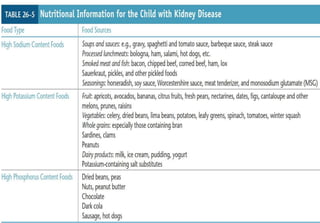
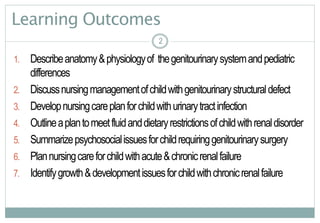
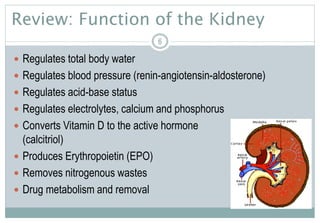
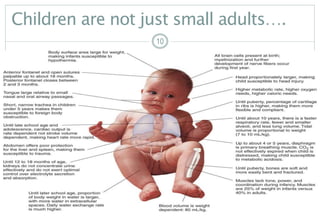
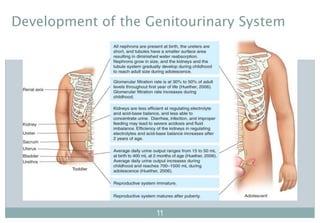
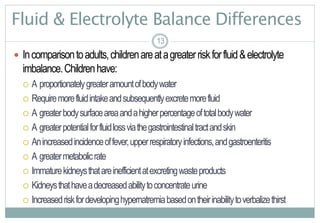
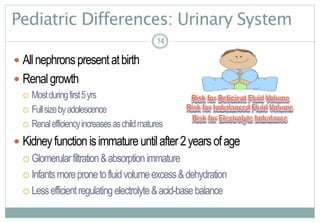
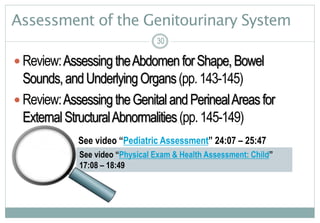
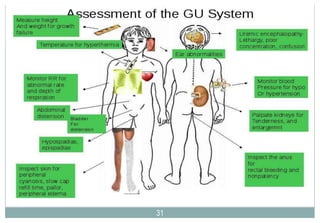
The document provides an overview of alterations in genitourinary function in children, including anatomy, development, common conditions like urinary tract infections, diagnostic tests, and treatment modalities. It reviews the differences between pediatric and adult genitourinary systems as well as important nursing considerations for assessing, diagnosing, and managing genitourinary issues in children.



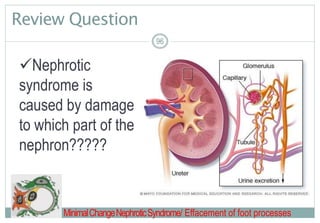
![50
Treatment Modalities
Urinarydiversion
Stents
Drainagetubes
Intermittent catheterization
Watchforlatexallergies
Pharmacologicalmanagement
Antibiotics
Anticholinergicforbladderspasm(oxybutynin[DitropanXL])
5050](https://image.slidesharecdn.com/alterationsingenitourinaryfunctioninchildren-161113204245/85/Alterations-in-genitourinary-function-in-children-50-320.jpg)