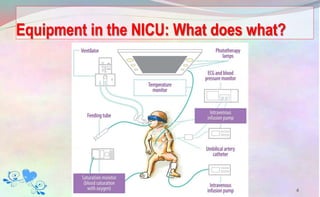
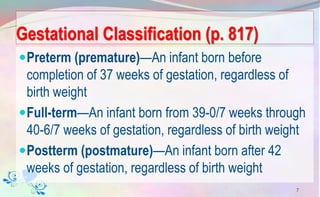
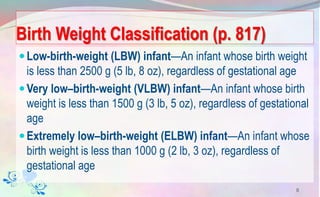
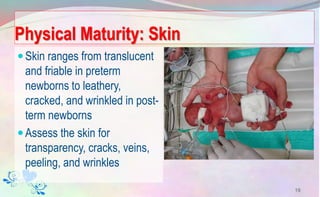
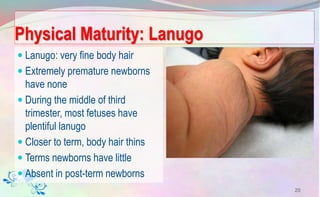
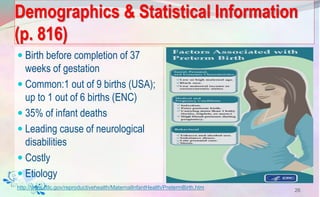
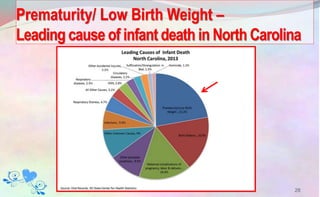
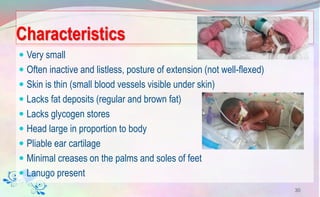
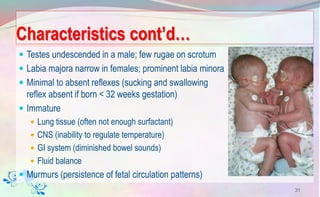
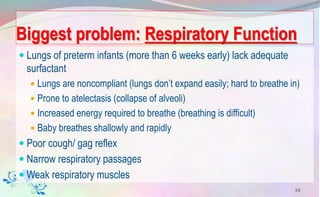
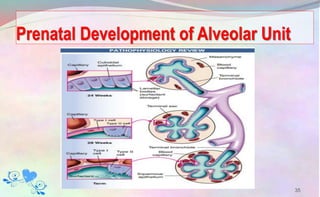
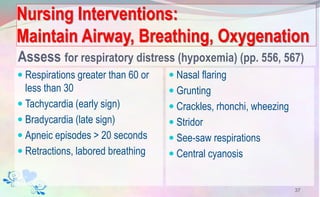
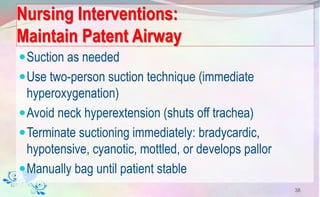
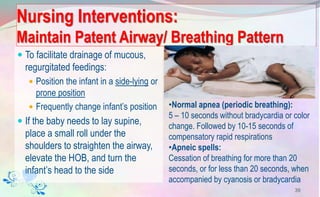
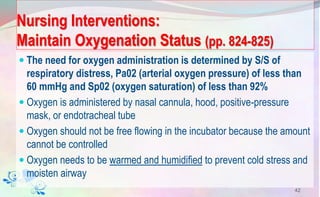
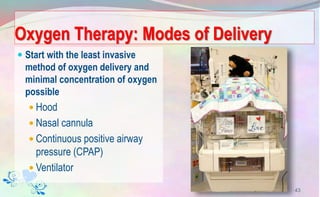
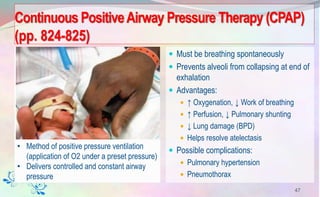
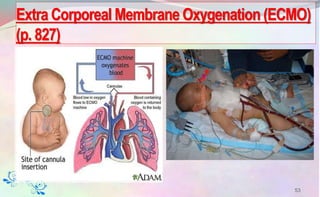
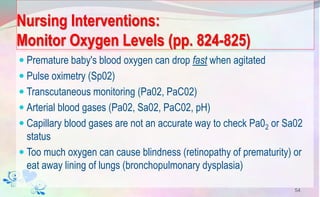
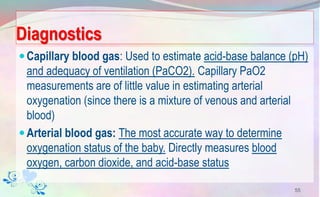
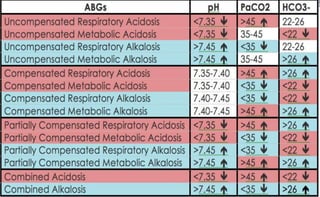
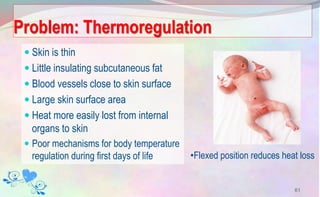
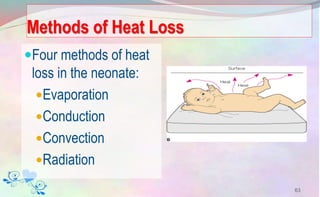
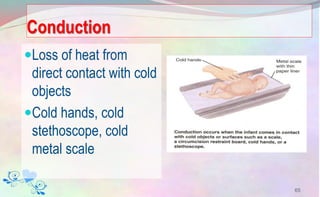
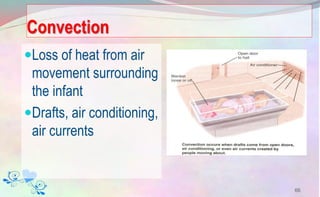
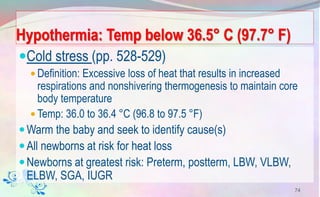
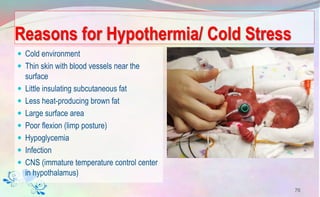
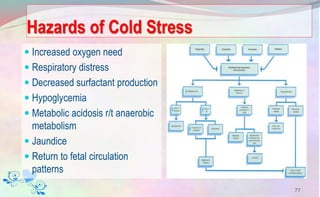
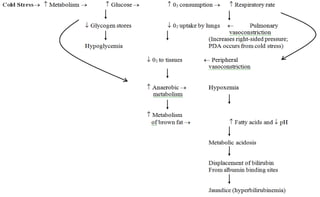
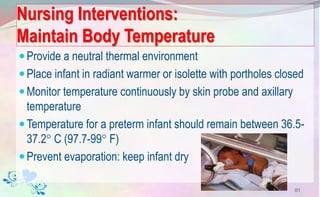
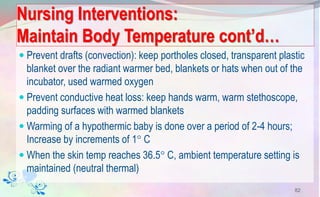
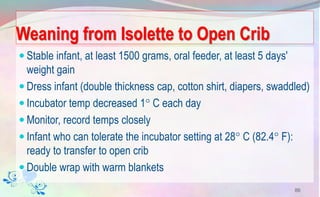
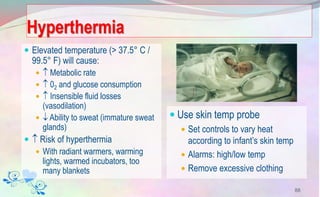
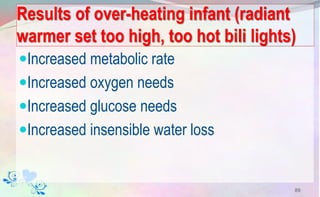
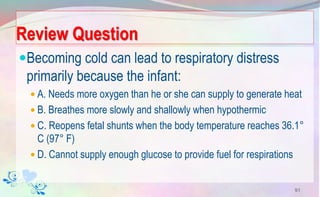
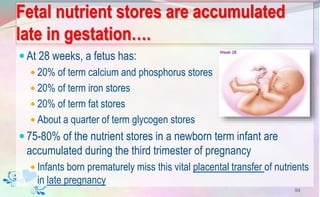
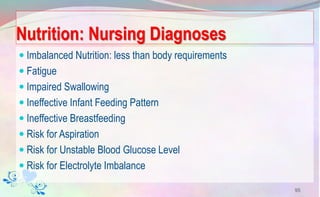
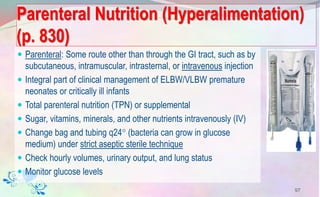
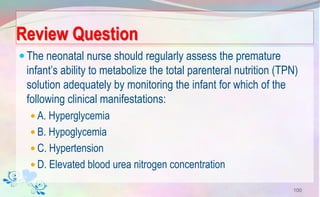
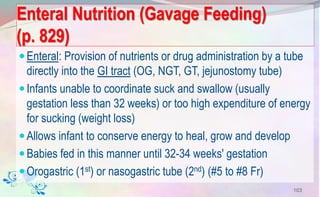
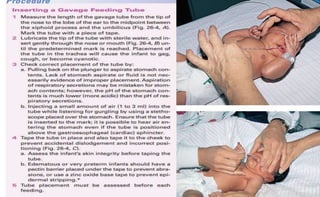
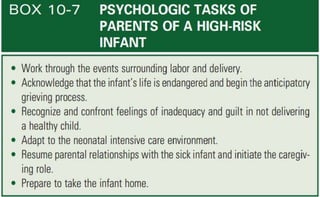
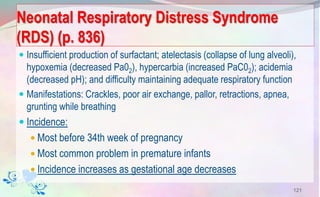
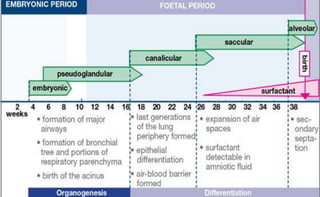
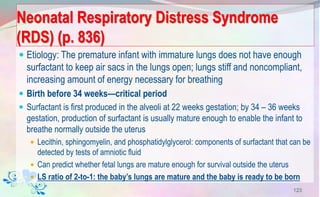
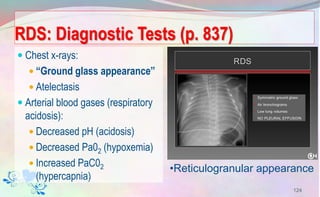
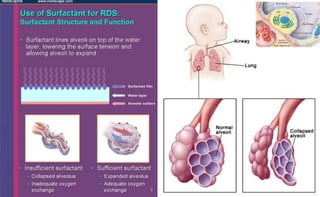
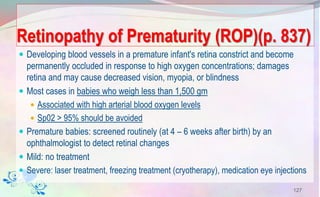
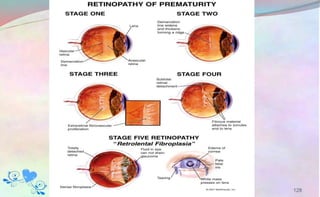
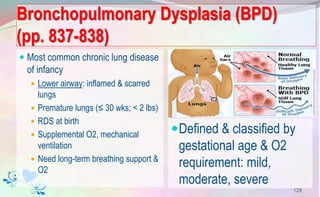
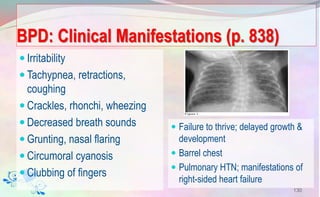
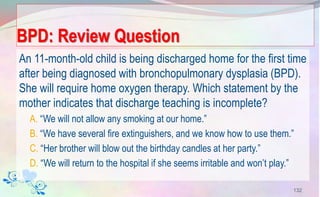
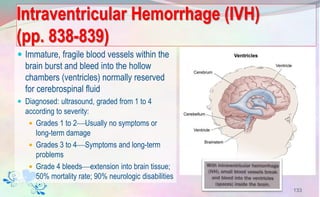
This document provides information on caring for preterm infants in the neonatal intensive care unit (NICU). It describes the characteristics of preterm neonates, including underdeveloped organs and difficulties with respiration, thermoregulation, and nutrition. The document outlines various respiratory conditions preterm infants may experience and discusses nursing interventions to maintain airway, breathing, and oxygenation. These include positioning, suctioning, oxygen therapy via various devices, surfactant administration, and other treatments. The goal is to support the preterm infant's immature systems and promote development until they can transition to extrauterine life.