This document provides information on health promotion for infants and toddlers. It outlines several objectives related to child development, nutrition, health concerns, communication, and anticipatory guidance. Nursing diagnoses that may be relevant for this age group are also listed. The document then reviews normal infant development by age group and describes common infant reflexes. It provides information on assessing growth, body systems, motor skills, language, vision, hearing, psychosocial development, sleep, and crib safety for infants.

![Review: Developmental Age Groups
(pp. 68 [new]; 81-82 [old], Ball & Bindler)
•Neonate: First 28 days of life
•Infancy: Birth to 1 year
•Toddler: 1 to 3 years
•Preschooler: 3 to 6 years
•School-ager: 6 to 12 years
•Adolescent: 12 to 18 years](https://image.slidesharecdn.com/healthpromotionoftheinfanttoddlerfall2017-170512174846/75/Health-promotion-of-the-infant-amp-toddler-fall-2017-4-2048.jpg)

























![Nystagmus & Strabismus
(pp. 447 [new]; 484; 490 [old], Ball & Bindler)
• Young infants lack eye coordination
• Transient nystagmus or strabismus
normal variant until 4 months
• Alignment of eye important due to
correlation with brain development
• Nystagmus: involuntary rapid eye
movements
• Treatment: eyeglasses, surgery of eye
muscles
• Strabismus: misaligned eyes
• Treatment: Surgical correction,
optometric vision training
• Untreated: can lead to amblyopia (lazy
eye) (p. 447 [new]; 519 [old]) 32
Normal: Reflections of light are symmetrical](https://image.slidesharecdn.com/healthpromotionoftheinfanttoddlerfall2017-170512174846/75/Health-promotion-of-the-infant-amp-toddler-fall-2017-32-2048.jpg)




![Infancy: Sleep
(pp. 159-160 [new];180 [old], Ball & Bindler)
• Newborn to 3 mos: 10 – 16 hours/ day
• Most infants begin to sleep for longer periods during the nights as they get
older
• Sleep patterns will be alternating the first year of life—sleep a lot at first, then
not sleeping as much
• Safe to Sleep Campaign—Helps prevent sudden infant death syndrome
(SIDS)
• Sudden, unexplained death of an infant younger than 1 yr old
• Fourth leading cause of death in infants < 12 mos
• “Safe to Sleep" campaign has reduced SIDS rate by 50%
http://www.nichd.nih.gov/health/topics/sids/Pages/default.aspx 39
See Risk Factors for SIDS (Box 20-3), p. 483 [new]; 529 [old]](https://image.slidesharecdn.com/healthpromotionoftheinfanttoddlerfall2017-170512174846/75/Health-promotion-of-the-infant-amp-toddler-fall-2017-39-2048.jpg)

![Safe Sleep Environment
(pp. 483-485 [new]; 528-529 [old], Ball & Bindler)
• Place infant on back to sleep, for naps and
at night
• Place infant on firm sleep surface (e.g.,
safety approved crib mattress with fitted
sheet)
• In parent’s room in a separate crib/ cradle/
bassinet (NOT sharing same sleeping
surface)
• NO soft surfaces (e.g., pillow, quilt,
sheepskin, or a waterbed)
• Keep soft objects out of infant’s sleep area
• No pillows or “fluffy” items in the crib (“Bare
is Best”) 41](https://image.slidesharecdn.com/healthpromotionoftheinfanttoddlerfall2017-170512174846/75/Health-promotion-of-the-infant-amp-toddler-fall-2017-41-2048.jpg)

![Apparent Life-Threatening Event (ALTE) (former term)
Brief Resolved Unexplained Event (BRUE) (recommended term)
(pp. 481-482 [new]; 527-528 [old], Ball & Bindler)
• Event that is frightening to the observer
• Infant younger than 1 yr
• Sudden, brief, less than 1 minute
• At least one of the following:
• Tone: Marked hypo- or hypertonia
• Respirations: Absent (apnea), decreased, or irregular
• Altered level of responsiveness
• Color: Cyanosis, pallor, or erythema
• Syndrome with a broad range of possible underlying causes
• Prematurity, GERD, pertussis, lower respiratory tract infections, sepsis, seizure, urinary tract
infection, child abuse/ Munchausen Syndrome by Proxy, miscellaneous
• Tx: thorough history of the event and careful physical examination, diagnostics, in-hospital
observation (to determine and then treat underlying cause); home cardiorespiratory monitor
44
See Home Care Instructions for the Infant Requiring a Cardiorespiratory Monitor (p. 482 [new], 528 [old])](https://image.slidesharecdn.com/healthpromotionoftheinfanttoddlerfall2017-170512174846/75/Health-promotion-of-the-infant-amp-toddler-fall-2017-44-2048.jpg)




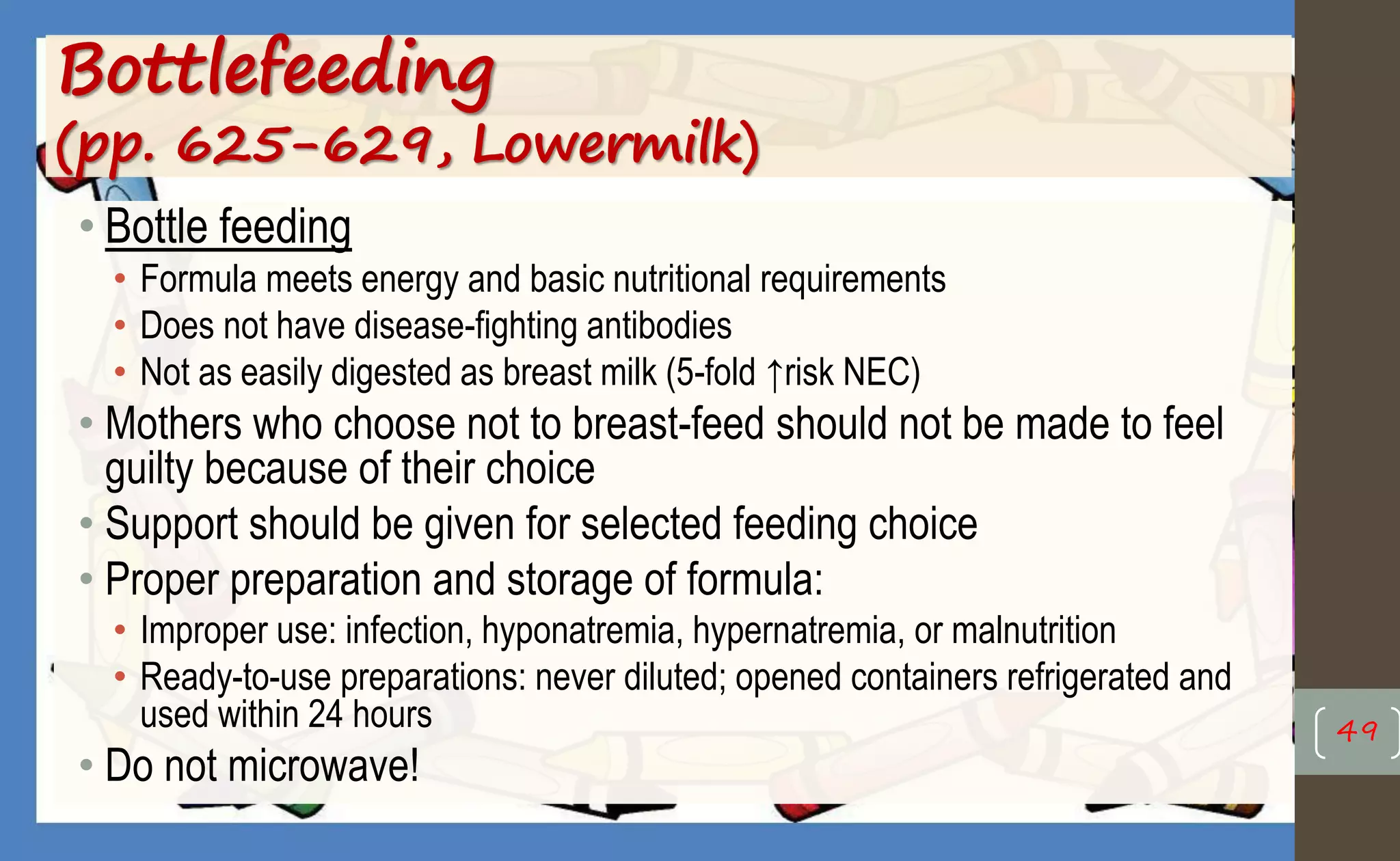


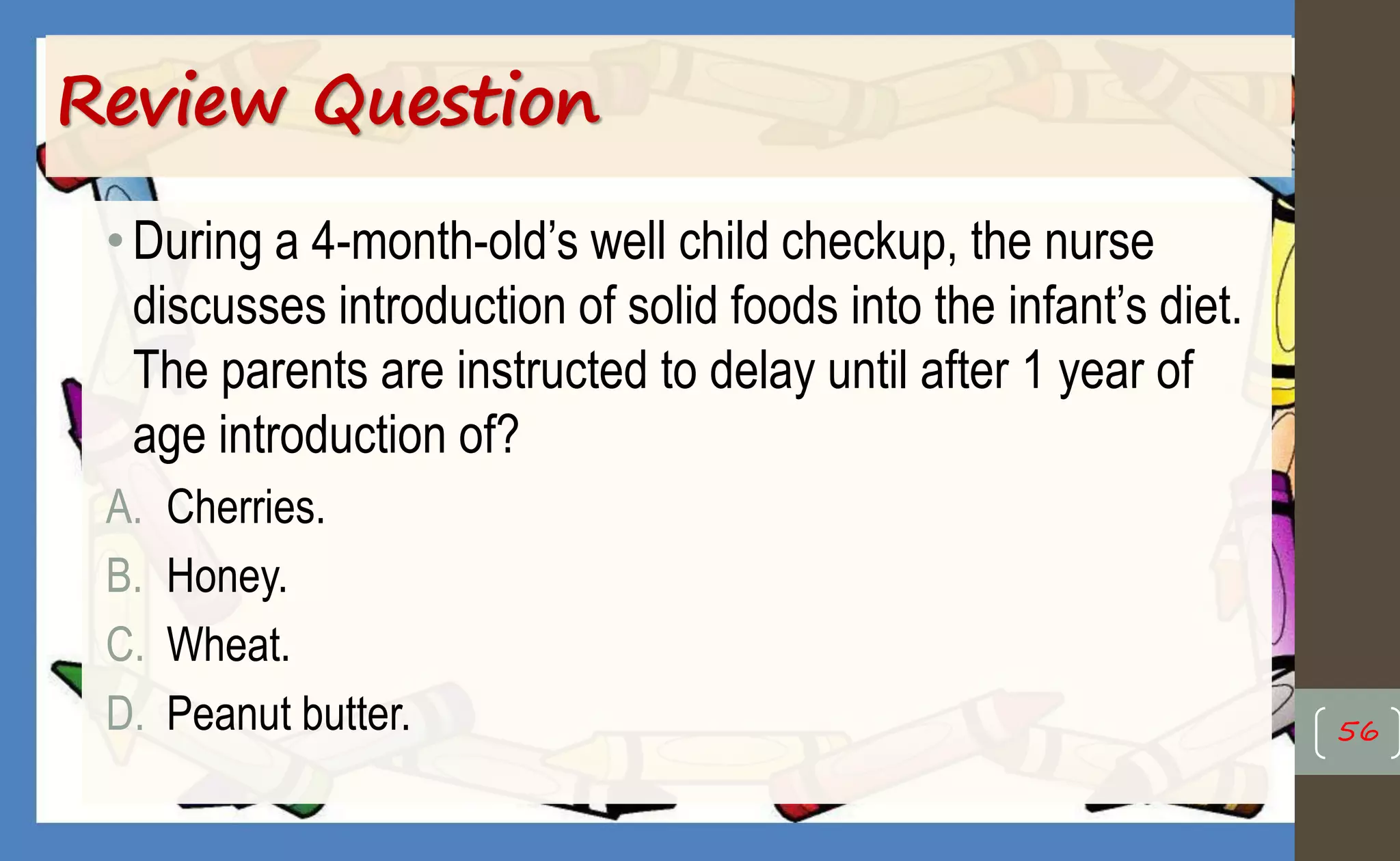
![Weaning and Solid Food Introduction
(Table 14-1, p. 284 [new], 317 [old])
• Weaning (6 to 12 months):
• NOT during stress; gradual: replacing one feeding at a time
• Solid Foods (4 to 6 months):
• Ready: can sit, extrusion reflex gone, can reach for objects and bring to mouth, can indicate
desire or refusal for food, and is able to safely move food to back of mouth and swallow
• Solids should be introduced one at a time in small amounts; wait at least 3 to 4 days before
introducing a new food; feed only from a spoon
• New recommendations: introduce peanut butter and other potential allergens at 4 to 6
months
• Any food, with the exception of honey and cow’s milk, can be introduced @ 4 to 6 months as long
as this is done one at a time to see if there is any reaction to each food
• It should be the right texture; make sure it is pureed
• Include ample amounts of fruits and vegetables
• Salt, sugar, and spices should not be added
• Food Allergies
• Abdominal pain, diarrhea, nasal congestion, wheezing, cough, vomiting, and rashes
52](https://image.slidesharecdn.com/healthpromotionoftheinfanttoddlerfall2017-170512174846/75/Health-promotion-of-the-infant-amp-toddler-fall-2017-52-2048.jpg)









![Safety
(REVIEW pp. 162-163 [new], 182-185 [old], Ball & Bindler)
• Accidental injury: The fifth leading cause of death during infancy
• Common causes: Suffocation and aspiration of small objects, motor vehicle crashes,
drowning, fire/ burns, poisoning, and falls (p. 7)
• Prevent asphyxiation—asphyxiation (suffocation) occurs when air cannot get into
or out of the lungs and oxygen supplies are depleted
• Choking: major concern in infancy and toddlerhood
• Keep small objects out of reach
• Cut food into small pieces; don’t let them have hard candy
• Substances or objects aspirated into airway
• Partial or complete obstruction of the lungs
• Strangulation: constriction of the neck; also blockage of nose & mouth by airtight
material
• All plastic bags or covers kept out of the infant’s reach
• NO latex balloons
65](https://image.slidesharecdn.com/healthpromotionoftheinfanttoddlerfall2017-170512174846/75/Health-promotion-of-the-infant-amp-toddler-fall-2017-65-2048.jpg)



![Toddler: Vital Signs & Physical
Characteristics
• HR: 80-120
• Respirations: 20-30
• BP: 88/45 (BP estimate: systolic 80 + [ 2x age]; diastolic 2/3s systolic)
• Affected by fever, dehydration, respiratory illnesses and drugs
• Measure BP at every provider’s office visit
• Physical Characteristics:
• Brain growing rapidly (good nutrition essential): 80% adult size by 2 yrs
• Whole milk (3.5%) until age 2, then 2% milk (need fat for brain development)
• Nervous system: continues to myelinate; fine motor control is refining
• Muscle tissue replacing adipose tissue (baby fat) present during infancy
• Gaining physical strength and ability
• Motor Development
• Gross Motor: refer to chart
• Fine Motor: refer to chart
70](https://image.slidesharecdn.com/healthpromotionoftheinfanttoddlerfall2017-170512174846/75/Health-promotion-of-the-infant-amp-toddler-fall-2017-70-2048.jpg)

![Toddler: Play & Language
• Parallel Play:
• Gross Motor:
• Ride-on toys; push and pull toys
• Fine Motor:
• Crayons--with supervision
• Tasks: fine & gross motor development
• Language (refer to chart): ability
developing rapidly
• RECEPTIVE SPEECH before
EXPRESSIVE SPEECH
• Tantrums (pp. 172-173 [new],193-194 [old]) 72](https://image.slidesharecdn.com/healthpromotionoftheinfanttoddlerfall2017-170512174846/75/Health-promotion-of-the-infant-amp-toddler-fall-2017-72-2048.jpg)


![Toddler: Psychosocial Development
• Erickson: Autonomy vs shame and doubt
• Autonomy--wanting to be in control. Conflict. Give them choices that are
appropriate
• Freud: Anal stage. Best example is toilet training; as their sphincters
become mature, they can assert control, autonomy over the bowel
• Moral development: Don’t know “right from wrong”
• No formed conscience: avoids punishment by controlling his or her behavior
• Right and wrong are determined by the consequences of actions
• Negativism: refer to "Toddler Characteristics”
• Temper tantrums--refer to "Toddler Characteristics;” p. 172 [new], 193 [old]
• Ritualism: refer to "Toddler Characteristics" 77](https://image.slidesharecdn.com/healthpromotionoftheinfanttoddlerfall2017-170512174846/75/Health-promotion-of-the-infant-amp-toddler-fall-2017-77-2048.jpg)

![Toddler
• Discipline:
• Role modeling (guiding behavior), ignoring, and/ or time out (placing
the child in a nonstimulating environment)
• Key ingredients: consistency, loving, immediate, realistic and age-
appropriate
• See Families Want to Know: Positive Discipline (p. 172 [new], 193 [old])
• Sibling rivalry:
• Make older child feel important, involved in care of younger sibling
• Safety is concern
• Constant supervision: Child < 3-1/2 yrs should never be left alone with infant 79](https://image.slidesharecdn.com/healthpromotionoftheinfanttoddlerfall2017-170512174846/75/Health-promotion-of-the-infant-amp-toddler-fall-2017-79-2048.jpg)


![Toddler Sensorimotor Phase, 1-2 yrs
(pp. 69-72 [new], 82-83 [old], Ball & Bindler)
• Learning by physical trial and error; imitate older children and adults
• Using all senses to explore environment; starting to think before
acting
• Rudimentary awareness of cause/ effect
• Rudimentary awareness of spatial relationships
• Object permanence--well established by toddler age
• Domestic mimicry--a toddler at this stage is often seen imitating the
parent of the same sex, performing household tasks
82](https://image.slidesharecdn.com/healthpromotionoftheinfanttoddlerfall2017-170512174846/75/Health-promotion-of-the-infant-amp-toddler-fall-2017-82-2048.jpg)
![Toddler Preoperational Phase, 2-4 yrs
(p. 72 [new], 83 [old], Ball & Bindler)
• ↑Understanding time and space
• ↑Use of language
• Mental trial and error rather than physical
• Problem solving based on what they see or hear
• Egocentrism: views everything in relation to self; unable to consider another's point of
view
• Transductive reasoning: reasoning from one particular fact or case to another similar
fact or case; unrealistic understanding cause-and-effect
• Magical thinking: feels extremely powerful; believes thoughts or wishes cause events to
happen
• Animism: believes that inert objects such as stuffed animals are alive and have wills of
their own
• Centration: ability to consider only one aspect of a situation at a time
• Irreversibility: cannot see a process in reverse order
83](https://image.slidesharecdn.com/healthpromotionoftheinfanttoddlerfall2017-170512174846/75/Health-promotion-of-the-infant-amp-toddler-fall-2017-83-2048.jpg)
![Toddler: Nutrition (p. 266 [new], 316 [old])
• Rate of growth/ appetite slows: "Physiologic Anorexia"
• Calorie requirements: 1300 calories/day (~ 100 kcal/ kg/ day)
• Prone to anemia
• Well-balanced meals. Small/ more frequent feedings. Allow healthy, nutritious
choices
• Avoid junk foods, non-nutrient foods, concentrated sweets, fats, fast foods
• Food jags: fixate on one food and want that food for an extended period of
time; usually passes with time
• Environment: sitting at table with family, minimal distractions (NO TV)
• Rest period before meal time to help increase appetite
• Do not give snacks to the child before meals
84](https://image.slidesharecdn.com/healthpromotionoftheinfanttoddlerfall2017-170512174846/75/Health-promotion-of-the-infant-amp-toddler-fall-2017-84-2048.jpg)


![Infant/ Toddler Dental Care
(pp. 116, 171-172 [new]; 133; 316 [old], Ball & Bindler)
• Deciduous teeth:
• Age 6-10 months: Eruption of first teeth
• 12 months: 6-8 teeth
• No teeth eruption by 12 months - think endocrine disorder
• Teething: cool liquids, cold teething rings, gentle gum massage
• Dental hygiene—use a soft washcloth
• Nonfluoridated toothpaste for children under age 2 (sodium fluoride is a potent
poison)
• Ages 2-5 yrs: pea-sized amount of fluoridated toothpaste per day, don’t allow to
swallow (must be carefully supervised)
• Fluoride drops (0.25 mg) recommended > 6 mos (with unfluoridated water)
• Dental fluorosis white spotted, yellow or brown stained and sometimes crumbly
teeth
88](https://image.slidesharecdn.com/healthpromotionoftheinfanttoddlerfall2017-170512174846/75/Health-promotion-of-the-infant-amp-toddler-fall-2017-88-2048.jpg)
![Deciduous Teeth Timeline
(p. 118 [new], 133 [old])
89
The first teeth begin to break through the gums at about 6 months of age. Usually, the
first two teeth to erupt are the two bottom central incisors (the two bottom front teeth).
Next, the top four front teeth emerge. After that, other teeth slowly begin to fill in,
usually in pairs -- one each side of the upper or lower jaw -- until all 20 teeth (10 in the
upper jaw and 10 in the lower jaw) have come in by the time the child is 33 months old.](https://image.slidesharecdn.com/healthpromotionoftheinfanttoddlerfall2017-170512174846/75/Health-promotion-of-the-infant-amp-toddler-fall-2017-89-2048.jpg)

![Early Childhood Caries
(“Baby Bottle Caries”) (p. 171 [new], 192 [old])
• One or more decayed, missing, or filled teeth
in children ages 71 months or younger
• 28% of young children
• Complications: abscess formation; need for
multiple teeth extractions
• Referrals: periodontics, orthodontics, oral surgery
• Painful, can hinder speech, delay development
• 19% experience interference with play, 32%
with school, 50% with sleeping, and 86% with
eating
• Tx: extraction of teeth under general anesthesia
(“Total Mouth Rehabilitation”)
• Prevention: Good oral hygiene practices;
avoid sweets; do NOT take bottle, sippy/
tippy cups to bed
91](https://image.slidesharecdn.com/healthpromotionoftheinfanttoddlerfall2017-170512174846/75/Health-promotion-of-the-infant-amp-toddler-fall-2017-91-2048.jpg)
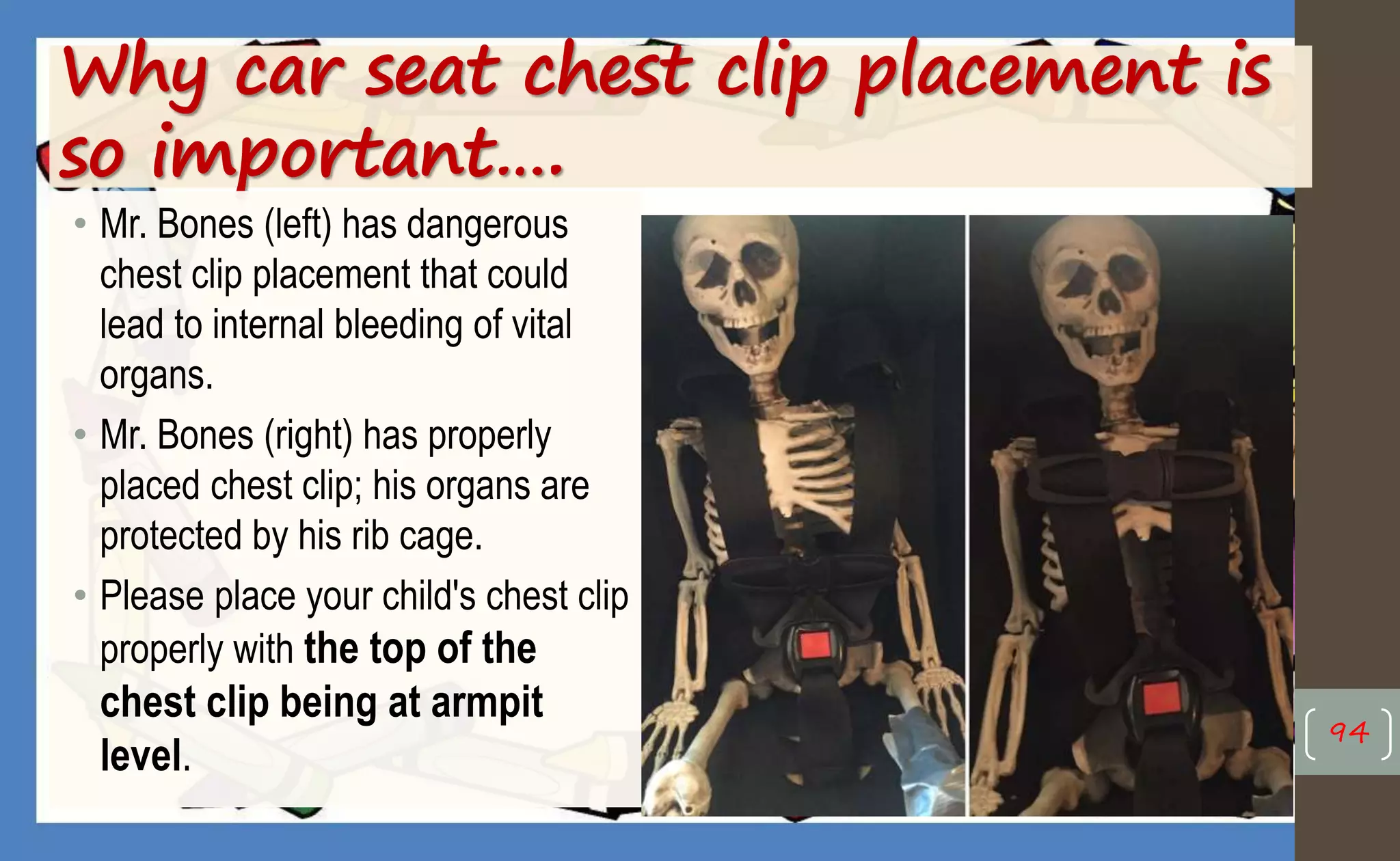
![Infant/Toddler: Car Safety
(p. 162, 176 [new]; 183, 197 [old])
• Car: Door locks
• Safety seats: http://www.buckleupnc.org/occupant-
restraint-laws/child-passenger-safety-law-summary/
• Children < 5 yrs, < 40 lbs restrained
in back seat (preferably center)
• Rear-facing child restraints for
children for a MINIMUM of 2 yrs &
reaches the highest weight/ height
allowed in the car seat
• When children outgrow rear-facing
seats: forward-facing car seats with
5-point harnesses until they reach
the upper weight or height limit of the
seat
92
Forward-facing (FF)
“toddler” / “combination”
seats are used only in the
forward-facing direction
and never for a child who
weighs less than 20 lbs or
is less than 2 yrs of age.
FF car seats generally fit a
child who weighs 20-40 lbs
or more and up to 40” tall.](https://image.slidesharecdn.com/healthpromotionoftheinfanttoddlerfall2017-170512174846/75/Health-promotion-of-the-infant-amp-toddler-fall-2017-92-2048.jpg)


![Toddler Safety
(pp. 175-176 [new]; 196-197 [old], Ball & Bindler)
• Fire and burns:
• No dangling cords from irons or
other small appliances
• Keep away from open fires and
heaters
• Electrical outlet covers
• Turn handles in on top of stove
• Water heaters 120 or less
• Preventing falls:
• Stairway gate
• Locks on doors and windows;
guards over screened windows
96](https://image.slidesharecdn.com/healthpromotionoftheinfanttoddlerfall2017-170512174846/75/Health-promotion-of-the-infant-amp-toddler-fall-2017-96-2048.jpg)
![Toddler Safety
(pp. 175-176 [new]; 196-197 [old], Ball & Bindler)
• Water safety:
• NEVER leave a child alone in water (can drown in 1” of water)
• Preventing poisoning:
• Locks on cabinets; child-resistant containers;
• “Mr. Yuk” stickers, Poison Control Center number by every telephone
(800-222-1222)
• Firearm safety:
• Keeping guns locked up and unloaded
97](https://image.slidesharecdn.com/healthpromotionoftheinfanttoddlerfall2017-170512174846/75/Health-promotion-of-the-infant-amp-toddler-fall-2017-97-2048.jpg)

![Toddler: Poisons
(pp. 175, 395-400 [new]; 433-436; 437-438 [old], Ball & Bindler)
• Poisoning – Ingestion of or exposure to toxic substances
• Children < 6 yrs more at risk due to developmental level
• Toddlers lack cognitive ability to know what is dangerous; caretakers need
to be on guard
• Most poisonings occur in the child’s home or homes of relatives or friends
• Most is oral ingestion: medications, household chemicals, cosmetics,
plants, and heavy metals
• Common toxic substances ingested by children include acetaminophen,
ibuprofen, aspirin, iron, hydrocarbons, corrosives, and/or lead
• Grandma’s purse: One pill can kill
99](https://image.slidesharecdn.com/healthpromotionoftheinfanttoddlerfall2017-170512174846/75/Health-promotion-of-the-infant-amp-toddler-fall-2017-99-2048.jpg)
![Toddler: Poisons
• Primary prevention is key: Avoiding Childhood Poisoning (p. 398 [new]; 436 [old])
• Keep medicines, vitamins and household products out of sight and
reach—locked is better than high
• NO syrup of Ipecac; call Poison Control Center (800-222-1222) or 911
• Decontamination strategies (Emergency Department): reverse toxicity by
giving an antidote (e.g., N-acetylcysteine, glucagon, naloxone); gastric
lavage (with life-threatening ingestions and within 60 minutes of ingestion;
must protect patient’s airway); gastric decontamination with activated
charcoal (1 g/ kg; often requires placement of NG tube); whole bowel
irrigation (prevents further absorption of sustained-release medications) 100
See “Clinical Manifestations: Commonly Ingested Toxic Agents,” p. 396 (new); 435 (old)](https://image.slidesharecdn.com/healthpromotionoftheinfanttoddlerfall2017-170512174846/75/Health-promotion-of-the-infant-amp-toddler-fall-2017-100-2048.jpg)
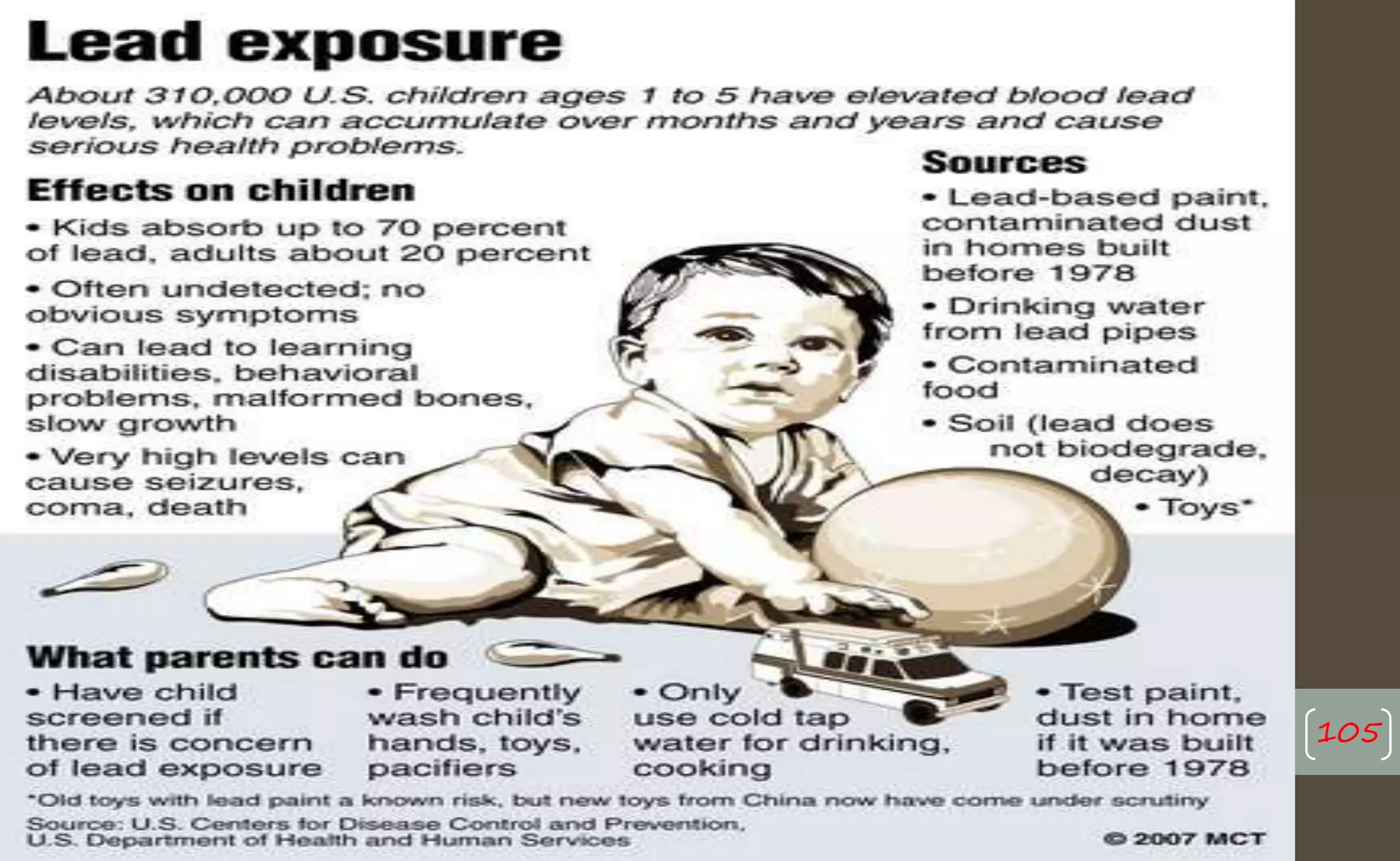
![Lead Poisoning
(pp. 399-400 [new]; 437-438 [old], Ball & Bindler)
• Ingestion, inhalation, or absorption through skin
• Primary source: deteriorating lead-based paint (structures built before 1978;
old toys/ from China, jewelry, and furniture coated with lead paint)
• Most harmful to children under the age of 6
• Lead affects every system of the body, ESPECIALLY the rapidly developing brain
and nervous system (causes irreversible CNS damage)
• Lead stored in the bones/ teeth; very difficult to remove from body (lead lines on
bones; blue-black gum lines)
• S/S: learning disabilities, developmental delays, decreased IQ scores, behavioral
problems (e.g., attention deficit hyperactivity disorder [ADHD], oppositional/conduct
disorders, & delinquency), seizures, hearing loss, malformed bones, slowed body
growth, loss of appetite, digestive issues, and kidney damage
• Anemia: lead interferes with the production of hemoglobin (↓ H & H) 101](https://image.slidesharecdn.com/healthpromotionoftheinfanttoddlerfall2017-170512174846/75/Health-promotion-of-the-infant-amp-toddler-fall-2017-101-2048.jpg)


![Lead Poisoning
(pp. 399-400 [new]; 437-438 [old], Ball & Bindler)
• Screening: 12 & 24 mos, or between 3-6 yrs
• Chelation therapy:
• Binds with lead, removes it from the blood (through urine and stool)
• Oral/ IV; dose/type depends on blood lead level (BLL)
• Edetate Calcium Disodium (CaNa2EDTA), dimercaprol (BAL), 2,3
Dimercaptosuccinic Acid (DMSA), penicillamine
• Many repeated doses required
• Long-term follow-up essential
• Remove lead hazards in child’s environment 104](https://image.slidesharecdn.com/healthpromotionoftheinfanttoddlerfall2017-170512174846/75/Health-promotion-of-the-infant-amp-toddler-fall-2017-104-2048.jpg)