This document provides an overview of nocturnal enuresis (bedwetting), including:
- Historical treatments included using animal organs or inducing blisters, with limited effectiveness. Psychic treatment in the 1920s showed an 87% success rate.
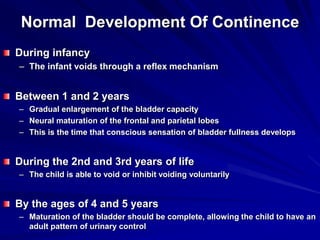
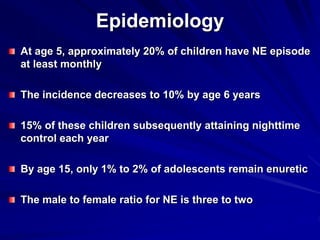
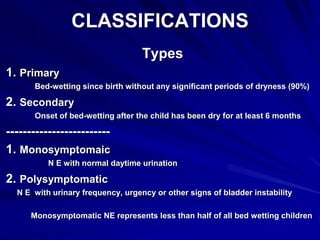
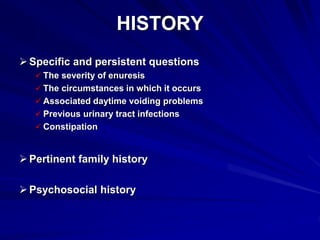
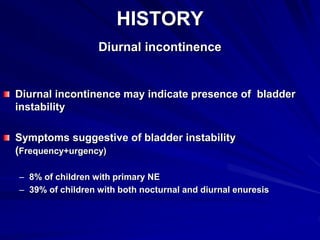
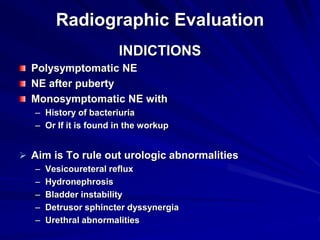
- Enuresis is usually due to a maturational delay and resolves naturally by age 15. Evaluation looks for underlying causes but most cases are primary nocturnal enuresis without other issues.
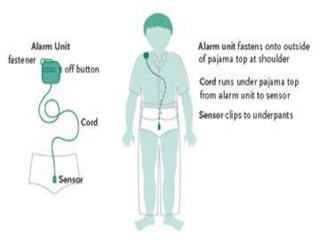
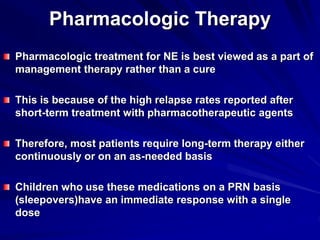
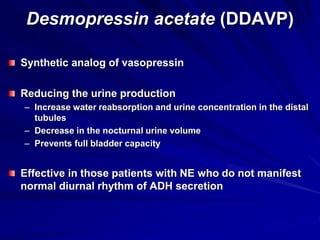
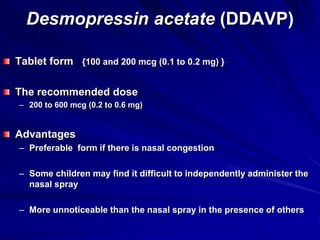
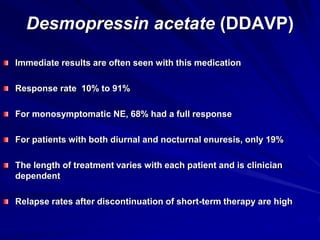
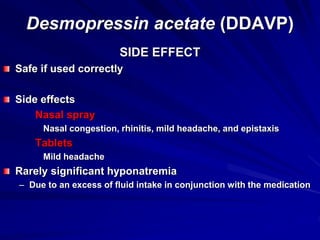
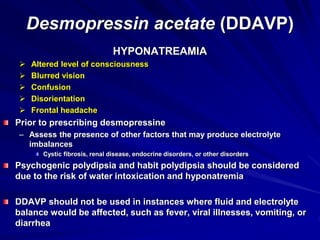
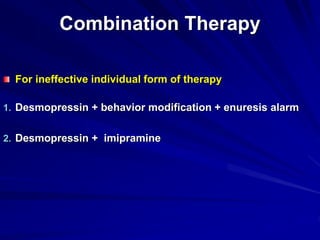
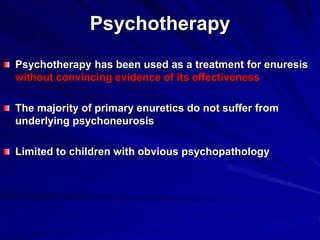
- Treatment focuses on education, behavioral modification using star charts and alarms, and pharmacotherapy like imipramine or desmopressin acetate. The goal is improving self-esteem until natural maturation occurs. A multimodal approach tailored to the