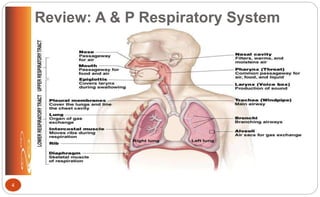
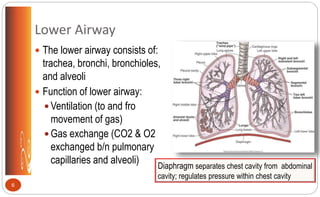
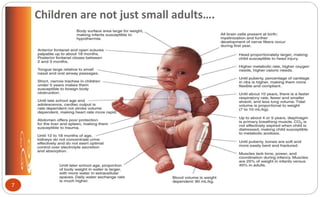
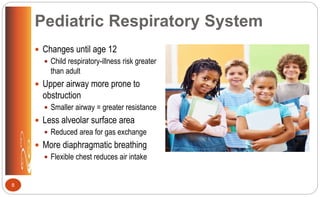
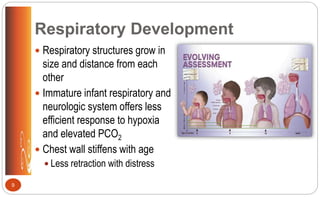
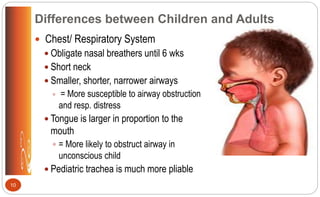
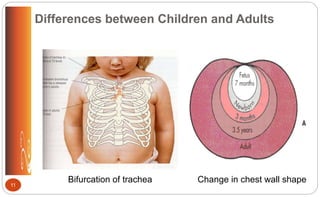
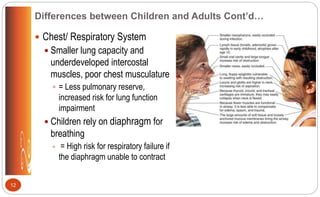
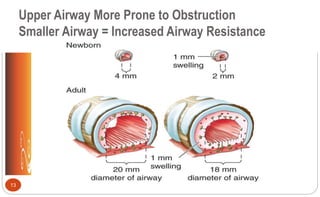
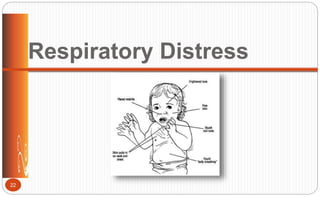
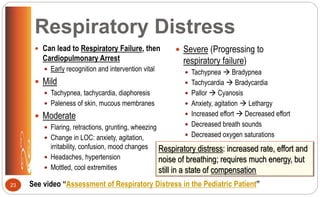
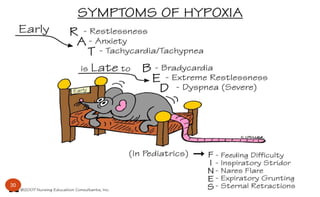
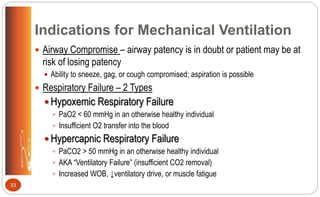
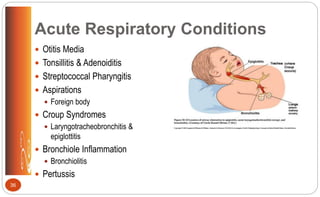
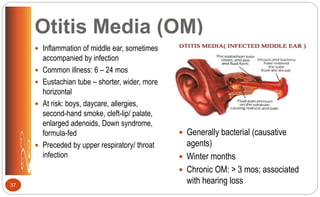
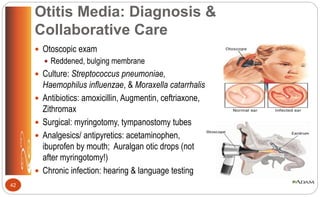
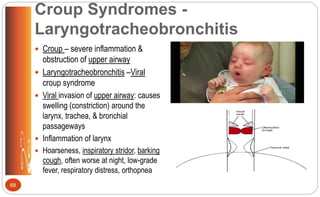
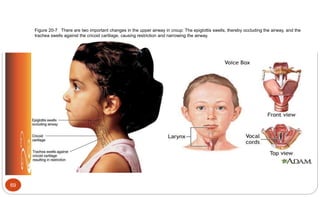
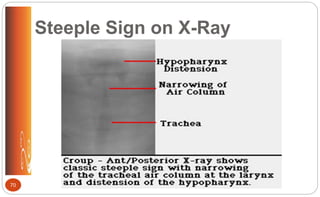
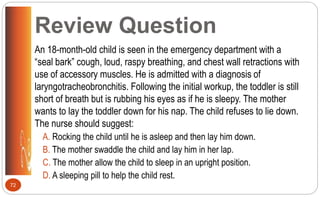
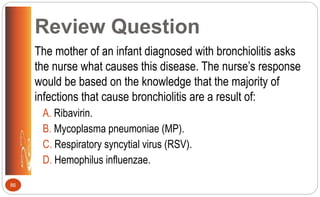
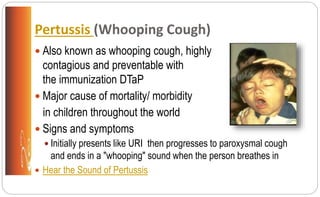
The document describes the anatomy and physiology of the pediatric respiratory system, key differences compared to adults, respiratory assessment in children, common acute respiratory conditions like otitis media, tonsillitis, and croup, signs of respiratory distress and failure, and nursing considerations for treatment and management of respiratory issues in children.
![Respiratory Assessment (p. 120 [new], 135 [old])
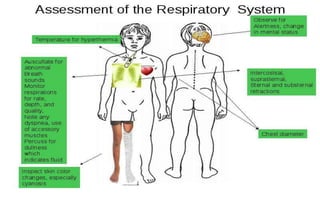
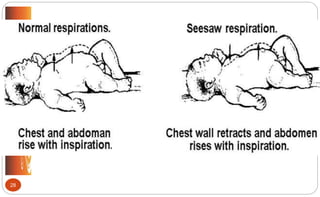
Inspection
Chest
Size, symmetry movement
Infancy shape is almost circular
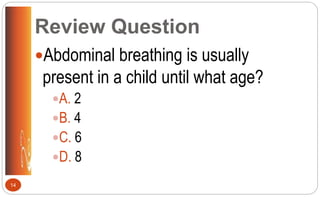
< 6-7 years respiratory
movement primarily abdominal
or diaphragmatic
Respirations
Rate, rhythm, depth, quality,
effort
> 60 /min in small children =
significant respiratory distress
16 See video “Pediatric Assessment” 22:03 – 23:18
•A consistent respiratory rate of less than
10 or more than 60 breaths/min in a child
of any age is abnormal and suggests the
presence of a potentially serious problem](https://image.slidesharecdn.com/respiratorylecturenurs3340fall2017-170515020529/85/Respiratory-lecture-nurs-3340-fall-2017-16-320.jpg)
![ Auscultation
Listen comparing one areas to
the other
Equality of breath sounds
Diminished
Poor air exchange
Abnormal breath sounds
Fine crackles
Wheezes (sibilant rhonchi)
Rhonchi (sonorous, coarse
crackles)
Stridor
Cough
* Prolonged inspiratory phase = upper
airway obstruction (croup, foreign body)
* Prolonged expiratory phase = lower
airway obstruction (asthma)
17
Respiratory Assessment (p. 122 [new], 138 [old])](https://image.slidesharecdn.com/respiratorylecturenurs3340fall2017-170515020529/85/Respiratory-lecture-nurs-3340-fall-2017-17-320.jpg)

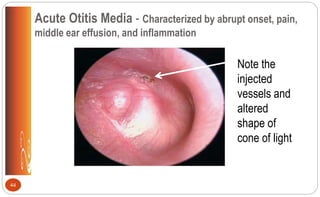
![Otitis Media: Clinical Manifestations
• Sudden piercing pain; irritability
• Fever (as high as 104°F [40°C])
• Vomiting, diarrhea
• Rubbing or pulling at ear
• Rolling head from side to side
• Night awakenings
• Muffled hearing; permanent
hearing loss
• Speech development problems
• Reddened, bulging membrane
40](https://image.slidesharecdn.com/respiratorylecturenurs3340fall2017-170515020529/85/Respiratory-lecture-nurs-3340-fall-2017-40-320.jpg)

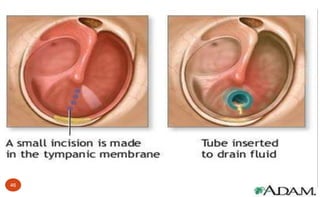
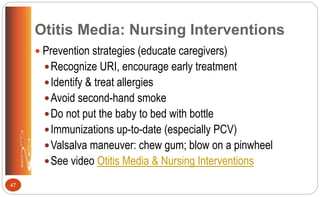
![Otitis Media: Nursing Interventions
General education:
Explain all diagnostic tests & procedures
Take full course of antibiotics
Warm compress, analgesics/ antipyretics
Positioning
Skin care
No cotton swabs
Comfort: relieve pain; facilitate drainage when possible; provide emotional
support to child & family
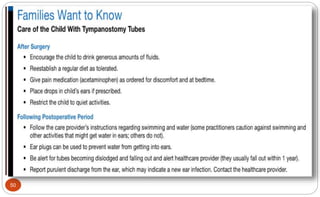
After surgery: “Care of the Child with Tympanostomy Tube” (p. 458 [new], 500 [old])
49](https://image.slidesharecdn.com/respiratorylecturenurs3340fall2017-170515020529/85/Respiratory-lecture-nurs-3340-fall-2017-49-320.jpg)

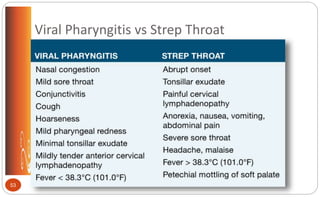
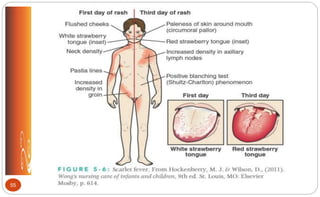
![Streptococcal Pharyngitis
Inflammation of structures in throat
School-aged children & teens
Symptoms strep throat: abrupt onset;
severe sore throat; painful cervical lymph
nodes; fever > 101° F (38.3° C); tonsillar
exudate; anorexia, nausea, vomiting,
abdominal pain; headache, malaise;
petechial mottling of soft palate; possible
scarlet rash (p. 469 [new], 512 [old])
Contrast: viral pharyngitis (p. 469 [new],
512 [old])
Dx: Rapid strep test, throat culture
Tx: 10-day course penicillin; may return
to school after 24 hrs of Tx
Complications: rheumatic fever,
rheumatic heart disease, and post-
streptococcal glomerulonephritis
Nursing interventions: plenty of rest &
fluids; sore throat symptom
management, prevent spread of
infection (same as for tonsillitis)
52](https://image.slidesharecdn.com/respiratorylecturenurs3340fall2017-170515020529/85/Respiratory-lecture-nurs-3340-fall-2017-52-320.jpg)





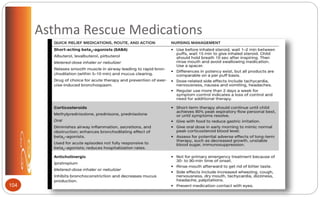
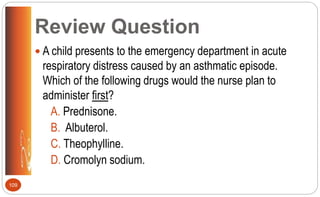
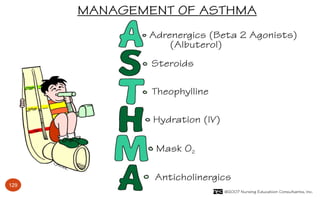
![Asthma: Rescue (Short-Term) Asthma
Control Medications (p. 499 [new], 544 [old])
Rescue medications
Short-acting beta agonists
(SABA) (bronchodilation, clear
mucous): albuterol (Ventolin);
levalbuterol (Xopenex); pirbuterol
(Maxair)
Anticholinergic (bronchodilation,
clear mucous): Ipratropium
(Atrovent)
Corticosteroids (anti-
inflammatory): prednisone;
prednisolone;
methylprednisolone
103](https://image.slidesharecdn.com/respiratorylecturenurs3340fall2017-170515020529/85/Respiratory-lecture-nurs-3340-fall-2017-103-320.jpg)
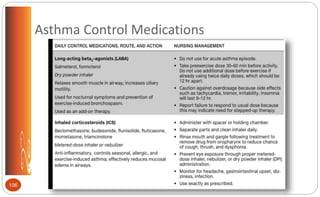
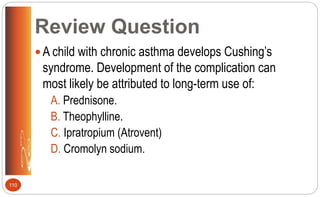
![Asthma: Long-term Asthma Control
Medications (pp.499-500 [new], 545 [old])
Long-acting beta-agonists (LABA) (bronchodilation): salmeterol (Serevent); formoterol
(Foradil, Perforomist)
Inhaled corticosteroids (ICS) (anti-inflammatory): beclomethasone (Qvar); budesonide
(Pulmicort); flunisolide (Aerobid); fluticasone (Flovent); mometasone (Asmanex);
triamcinolone (Azmacort)
Leukotriene receptor antagonist (LTRA) (bronchodilation, anti-inflammatory): montelukast
(Singulair); zafirlukast (Accolate); zileuton (Zyflo)
Mast-cell inhibitors (anti-inflammatory): cromolyn sodium (Intal); nedocromil (Tilade)
Theophylline (bronchodilation)
Combination inhalers (bronchodilation, anti-inflammatory): fluticasone-salmeterol (Advair
Diskus), budesonide-formoterol (Symbicort) and mometasone-formoterol (Dulera)
105 See video Respiratory Meds](https://image.slidesharecdn.com/respiratorylecturenurs3340fall2017-170515020529/85/Respiratory-lecture-nurs-3340-fall-2017-105-320.jpg)




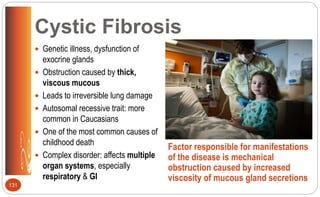
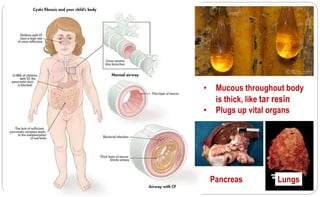
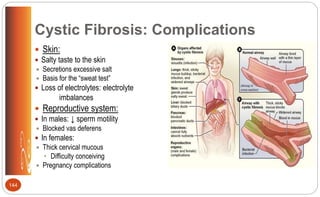
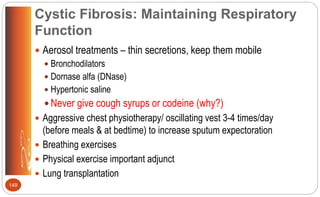
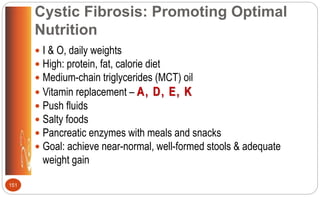

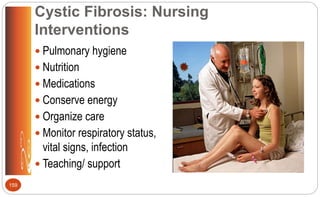
![Cystic Fibrosis: Medications (p.509 [new], 558 [old])
Aerosol bronchodilators to open airways
Mucolytic enzyme (Dornase alfa [Pulmozyne]) – to thin mucous to cough it
out easier
Mist of hypertonic saline – to clear thick mucous from lungs
Ibuprofen – slows lung function decline
Inhaled antibiotics (tobramycin) – antimicrobial for chronic lung infections
(Pseudomonas aeruginosa)
Oral and IV antibiotics – treat and suppress infections
Pancreatic enzymes to help digest food
Vitamins A, D, E, K / fat soluble vitamins
158](https://image.slidesharecdn.com/respiratorylecturenurs3340fall2017-170515020529/85/Respiratory-lecture-nurs-3340-fall-2017-158-320.jpg)