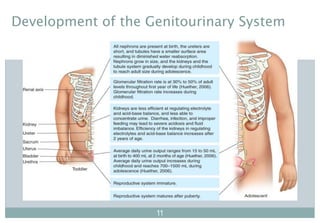
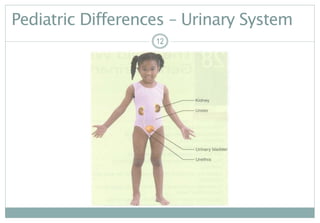
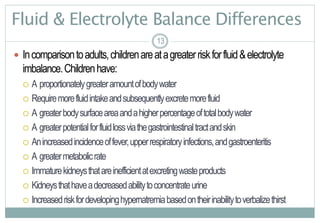
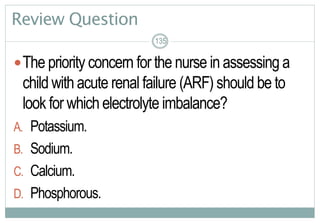
This document provides an overview of the anatomy, physiology, development, and common issues related to the pediatric genitourinary system. It begins with learning outcomes and then reviews anatomy and physiology of the urinary system and kidneys. It describes differences in fluid balance, renal function, bladder capacity, and reproductive system development in children compared to adults. The document outlines topics to include in a health history and physical assessment for the genitourinary system. It lists common nursing diagnoses and diagnostic tests used to evaluate the system.


![30
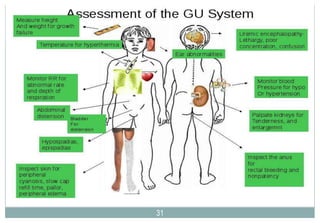
Assessment of the Genitourinary System
Review:AssessingtheAbdomenforShape,Bowel
Sounds,andUnderlyingOrgans(pp.127-128[new],143-145[old])
Review:AssessingtheGenitalandPerinealAreasfor
ExternalStructuralAbnormalities(pp.128-130[new],145-149[old])
30
See video “Pediatric Assessment” 24:07 – 25:47
See video “Physical Exam & Health Assessment: Child”
17:08 – 18:49](https://image.slidesharecdn.com/alterationsingenitourinaryfunctioninchildrenfall2017-170515232953/85/Alterations-in-genitourinary-function-in-children-fall-2017-30-320.jpg)

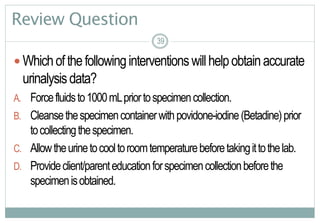
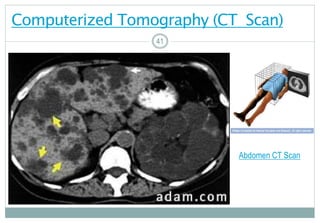
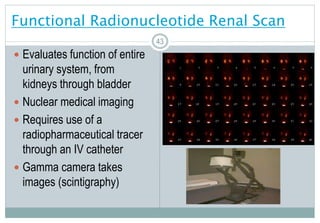
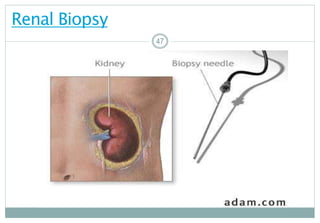
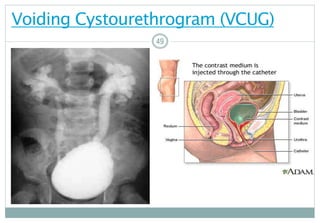
![40
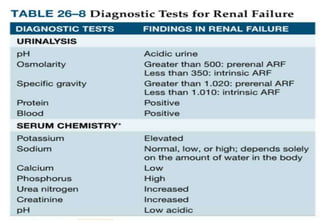
Diagnostic Tests (p. 704 [new], 766 [old])
ComputedTomography(CT)
Cystoscopy
FunctionalRadionucleotideRenalScan
IVP–IntravenousPyelogram
RenalBiopsy
RenalorBladderUltrasound
VCUG–VoidingCystourethrogram
4040](https://image.slidesharecdn.com/alterationsingenitourinaryfunctioninchildrenfall2017-170515232953/85/Alterations-in-genitourinary-function-in-children-fall-2017-40-320.jpg)
![50
Treatment Modalities
Urinarydiversion
Stents
Drainagetubes
Intermittent catheterization
Watchforlatexallergies
Pharmacologicalmanagement
Antibiotics
Anticholinergicforbladderspasm(oxybutynin[DitropanXL])
5050](https://image.slidesharecdn.com/alterationsingenitourinaryfunctioninchildrenfall2017-170515232953/85/Alterations-in-genitourinary-function-in-children-fall-2017-50-320.jpg)

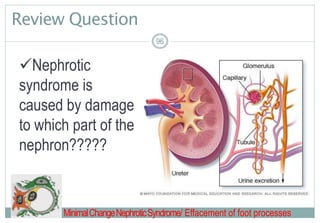
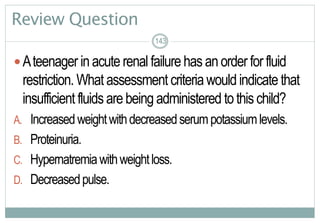
![97
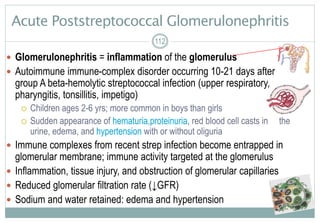
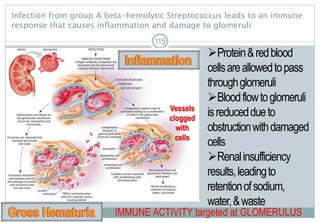
Contrast Between Normal Glomerular Anatomy &
Changes of Nephrotic Syndrome (p. 713 [new], 818 [old])
97
Massiveamountsofproteinare
excretedinurine
Edemaresultsfromdecreased
oncoticplasmapressure,renin-
angiotensin-aldosteroneactivation,&
antidiuretichormonesecretion
Loweralbuminbloodlevel
stimulatesthelivertogeneratelipids
&excessiveclottingfactors
Loss of podocyte foot processes = MASSIVE PROTEINURIA](https://image.slidesharecdn.com/alterationsingenitourinaryfunctioninchildrenfall2017-170515232953/85/Alterations-in-genitourinary-function-in-children-fall-2017-97-320.jpg)

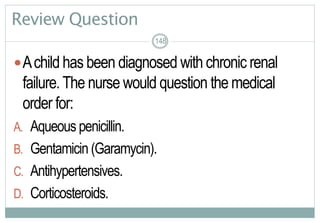
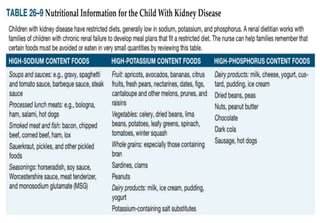
![Chronic Real Failure: Collaborative Care
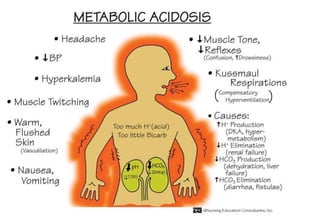
Dx:BUN/serumcreatinine(mostimportanttests);serumelectrolytes,
bicarbonate;CBC;urinalysis(proteinuria,hematuria,pyuria,sp.gravity,hyaline
casts);estimationofGFR;US/radionuclidestudies;renalbiopsy
Treatmentdependsoncourseofthedisease
Medications -seechart,p.723(new),787(old)
Diettherapy–limit potassium,phosphorus,sodium(seeTable26-9,p.724[new],788{old})
Proteinrestrictedonlytotherecommendeddailyallowanceforchildren
Preventionandtreatmentofcomplicationsofdecreasedkidneyfunction(e.g.,anemia,bonedisease,
cardiovascularmanifestations,hypertension,growthfailure)
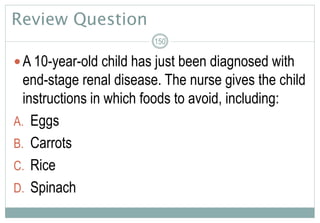
Avoidnephrotoxicmedications(NSAIDs.,radiocontrastagents,aminoglycosideabx)
Renalreplacementtherapy,ifsigns/symptomsofuremiaarepresent
Regularlifelongfollow-up
146](https://image.slidesharecdn.com/alterationsingenitourinaryfunctioninchildrenfall2017-170515232953/85/Alterations-in-genitourinary-function-in-children-fall-2017-146-320.jpg)