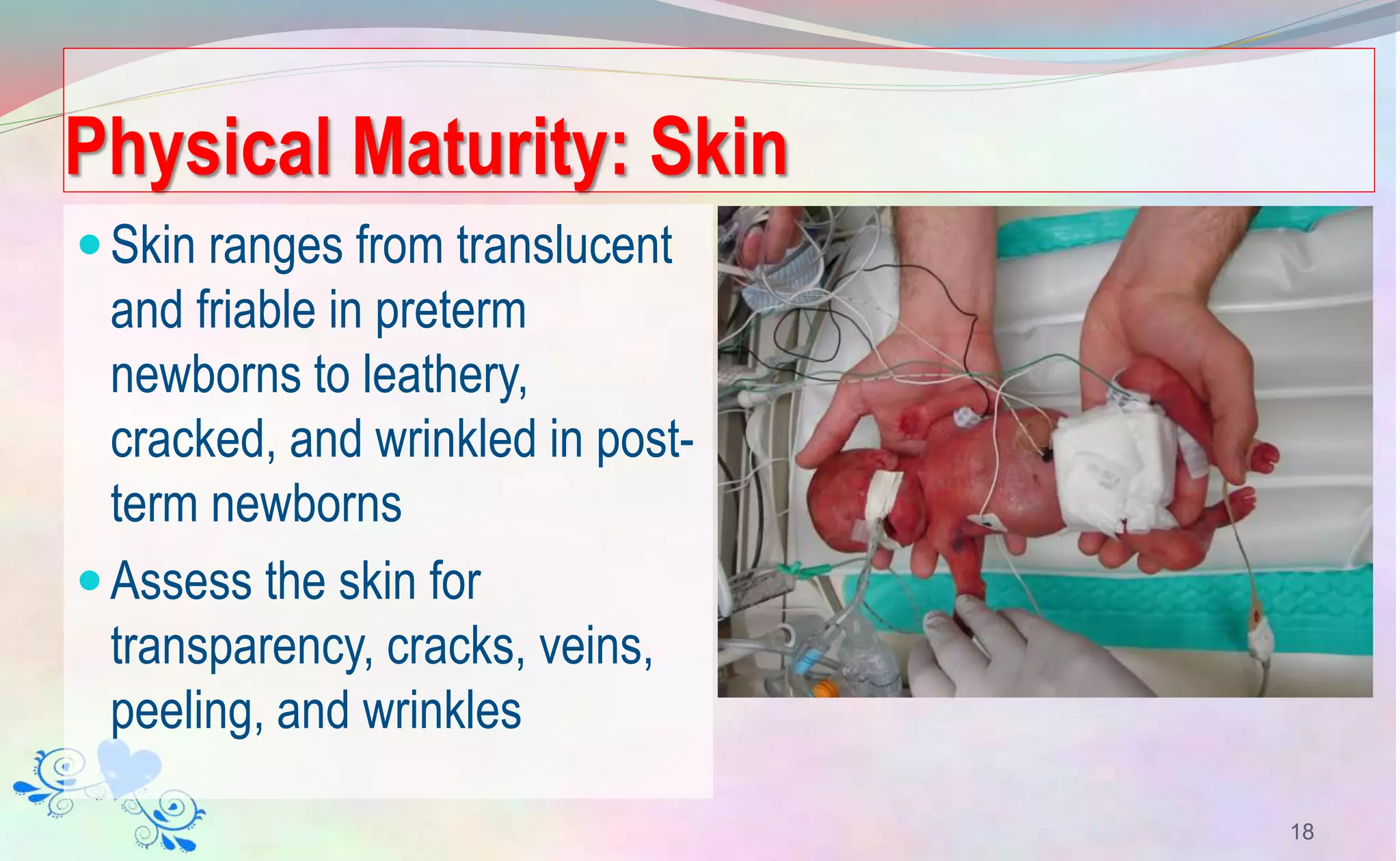
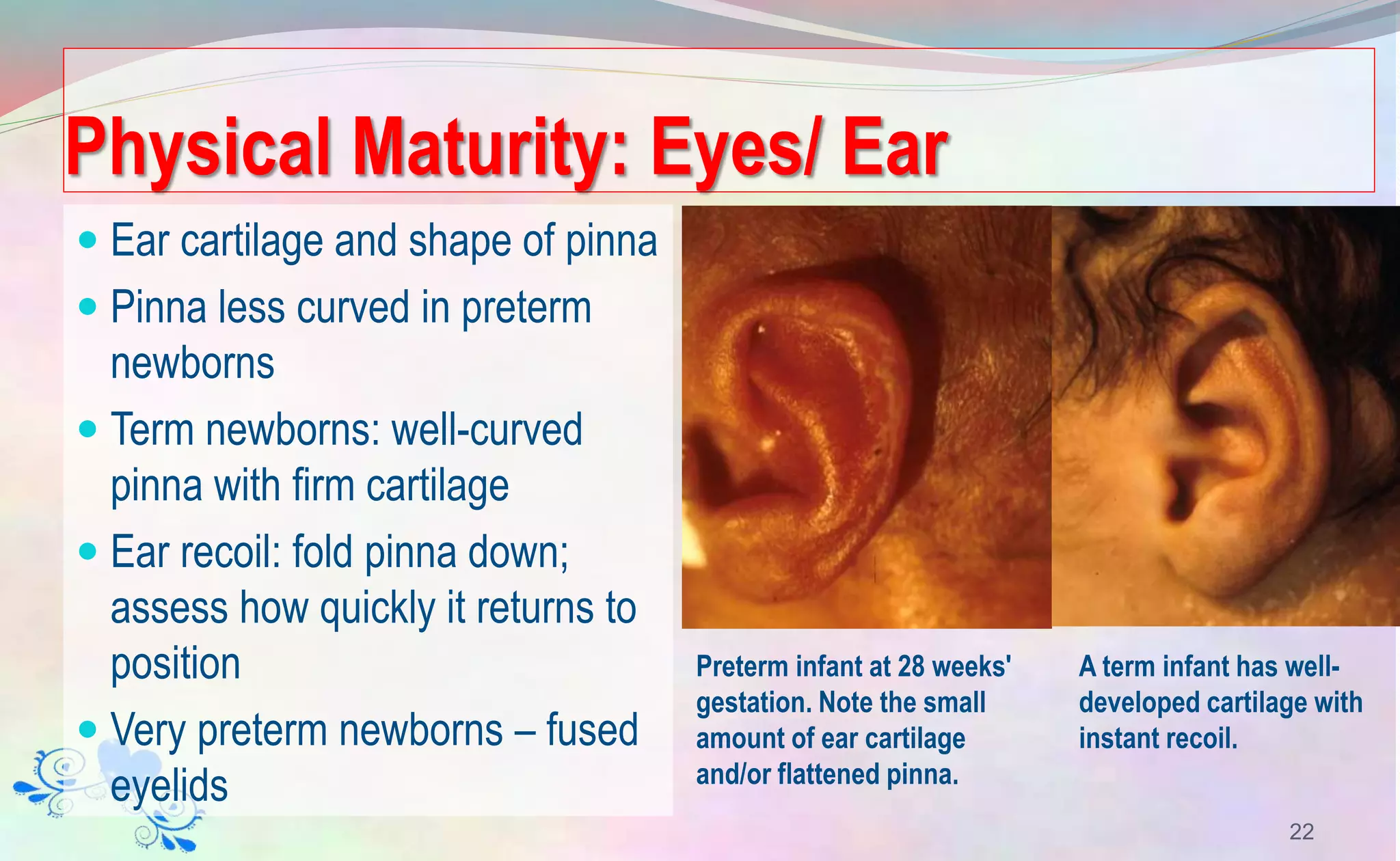
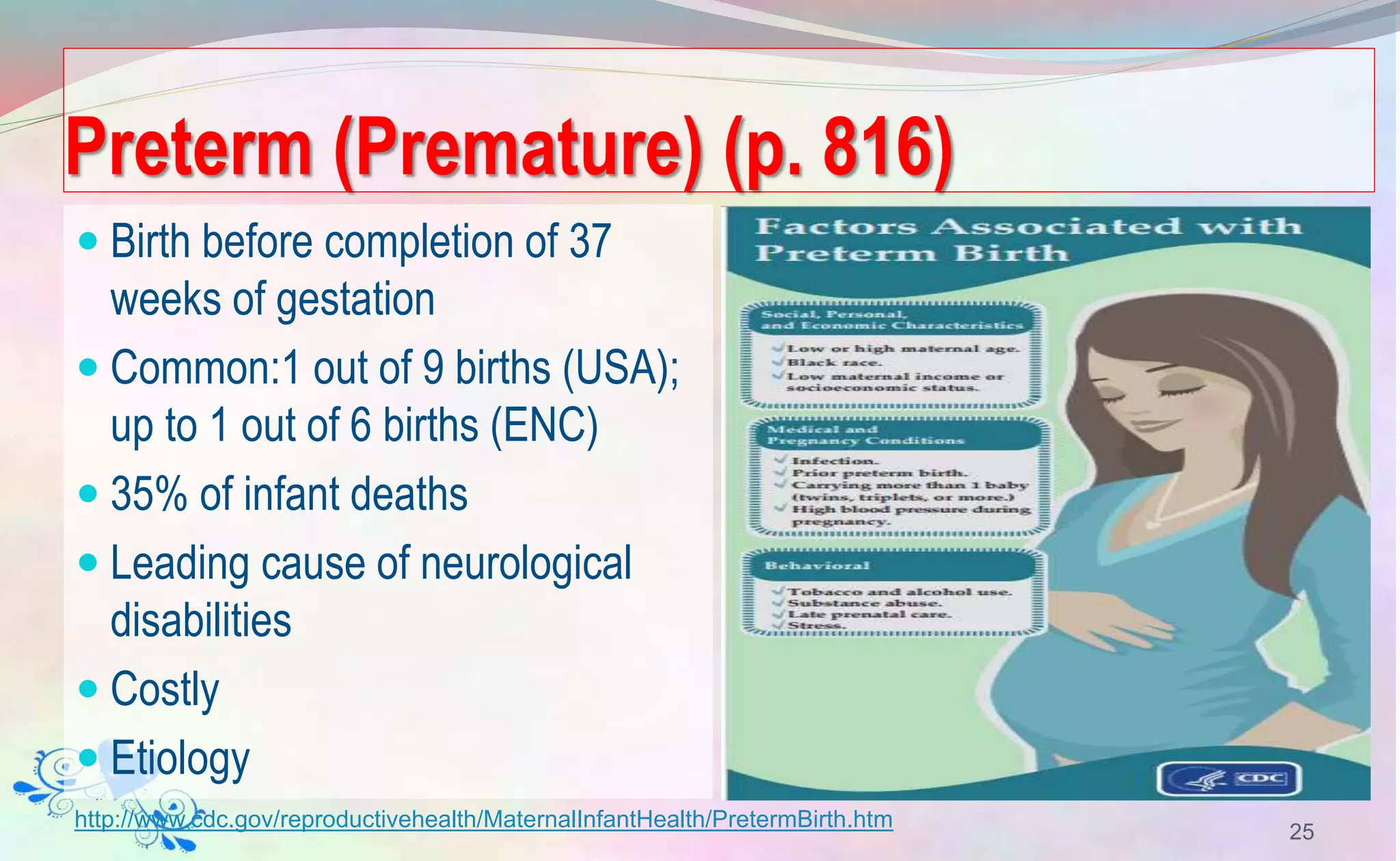
This document provides information on caring for preterm infants in the neonatal intensive care unit (NICU). It begins by describing the characteristics of preterm neonates, noting their underdeveloped organs and difficulties with respiration, thermoregulation, and nutrition. The document then discusses various respiratory conditions common in preterm infants, such as respiratory distress syndrome, and outlines nursing care to maintain the infant's airway, breathing, and oxygenation. This includes positioning, suctioning, monitoring oxygen levels, and potential supplemental oxygen therapies or mechanical ventilation if needed.