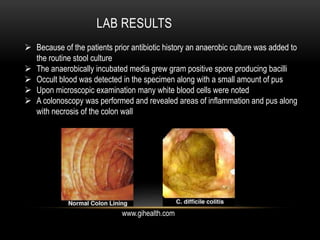
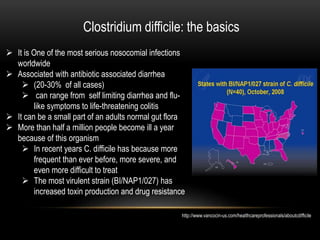
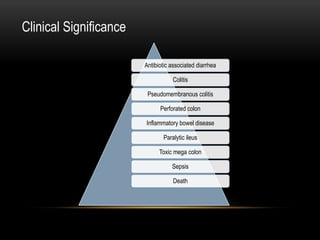
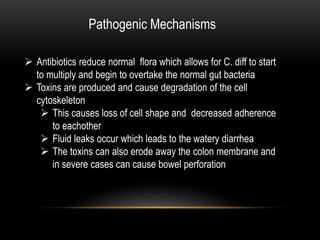
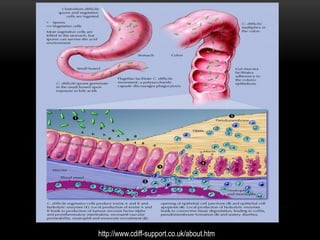
This patient, a 67-year-old female, presented with watery diarrhea, abdominal pain, fever, nausea and loss of appetite. She had recently taken antibiotics for a urinary tract infection. Stool tests found Clostridium difficile, confirming a diagnosis of pseudomembranous colitis. C. difficile infection is associated with antibiotic use and can cause symptoms ranging from diarrhea to life-threatening inflammation of the colon. The patient was likely infected due to her prior antibiotic treatment and hospital stay.