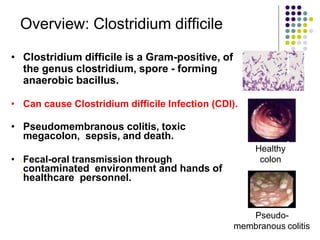
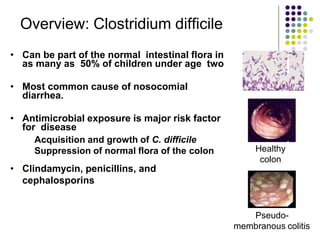
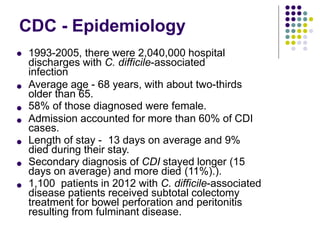
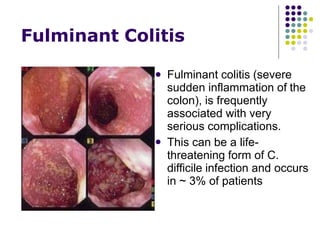
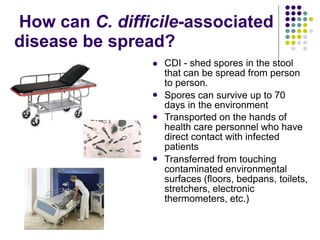
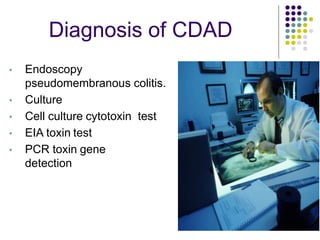
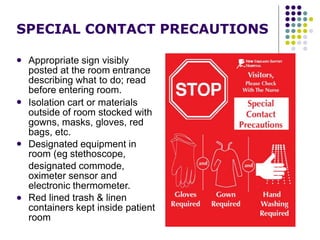
Clostridium difficile is a spore-forming, toxin-producing bacterium that can cause severe diarrhea and life-threatening complications. It is commonly acquired in healthcare settings due to antibiotic use disrupting the normal gut flora. Symptoms range from watery diarrhea to pseudomembranous colitis. Diagnosis involves toxin detection in stool samples. Treatment focuses on antibiotic therapy and infection control measures to limit transmission.