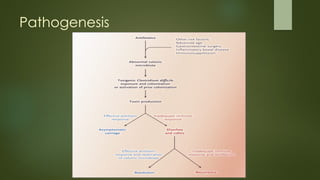
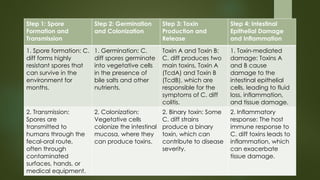
Clostridium difficile (C. difficile) is a spore-forming bacterium that causes severe gastrointestinal issues, particularly colitis, often following antibiotic use. This document outlines the bacterium's epidemiology, morphology, causes of infection, symptoms, risk factors, diagnosis, treatment, prevention, and complications associated with C. difficile, highlighting the importance of antibiotic stewardship and hygiene in managing outbreaks. Additionally, it addresses recurrence and the potential role of fecal microbiota transplantation in treating recurrent infections.