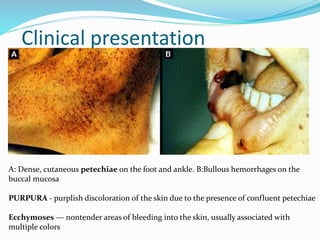
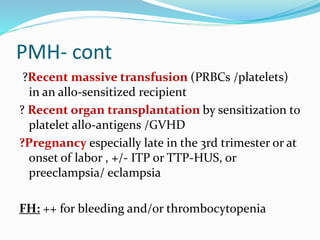
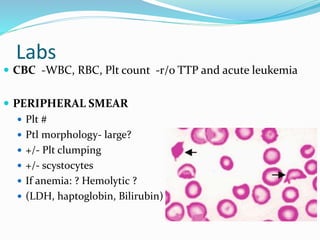
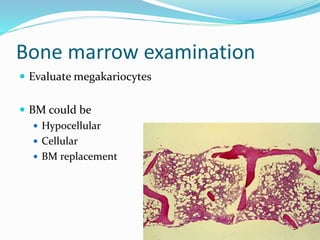
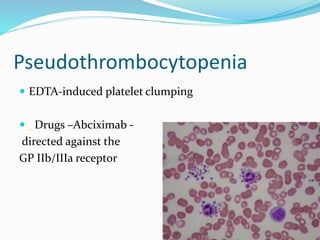
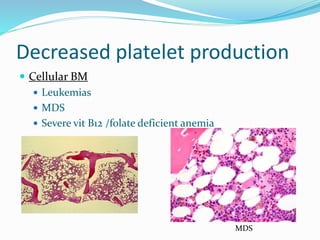
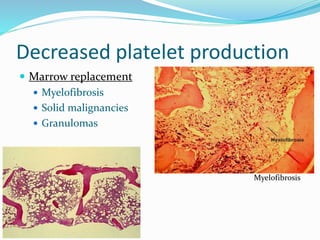
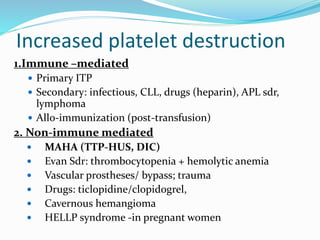
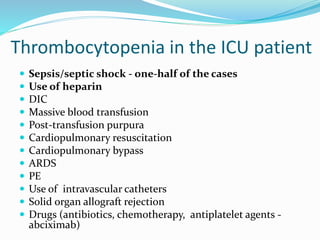
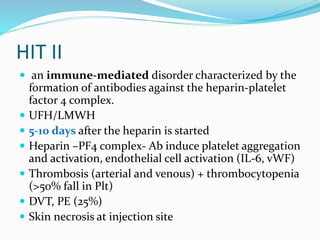
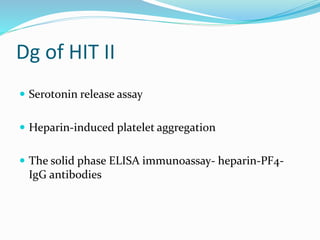
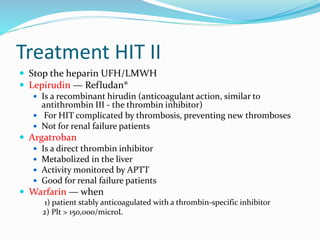
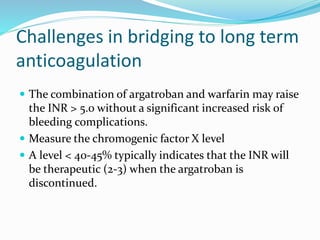
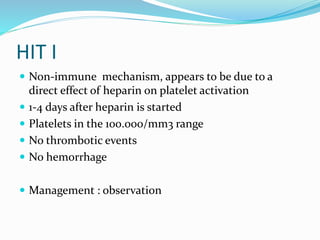
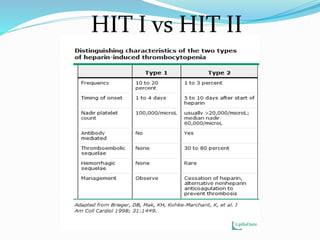
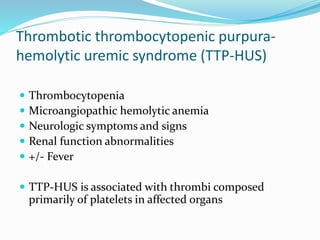
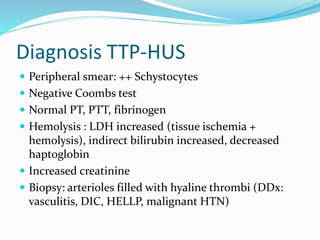
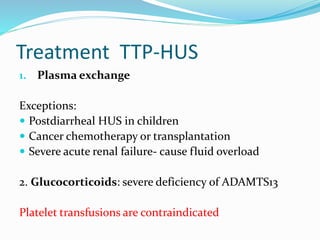
This document provides definitions and information about thrombocytopenia (platelet count <150,000/ml). It discusses increased bleeding risk with very low platelet counts and common clinical presentations. Potential causes of thrombocytopenia include decreased platelet production, increased platelet destruction, dilutional effects, and pseudothrombocytopenia. Specific conditions covered in detail include immune thrombocytopenic purpura, heparin-induced thrombocytopenia, thrombotic thrombocytopenic purpura-hemolytic uremic syndrome. Evaluation, diagnosis, and treatment approaches are outlined for the different conditions.