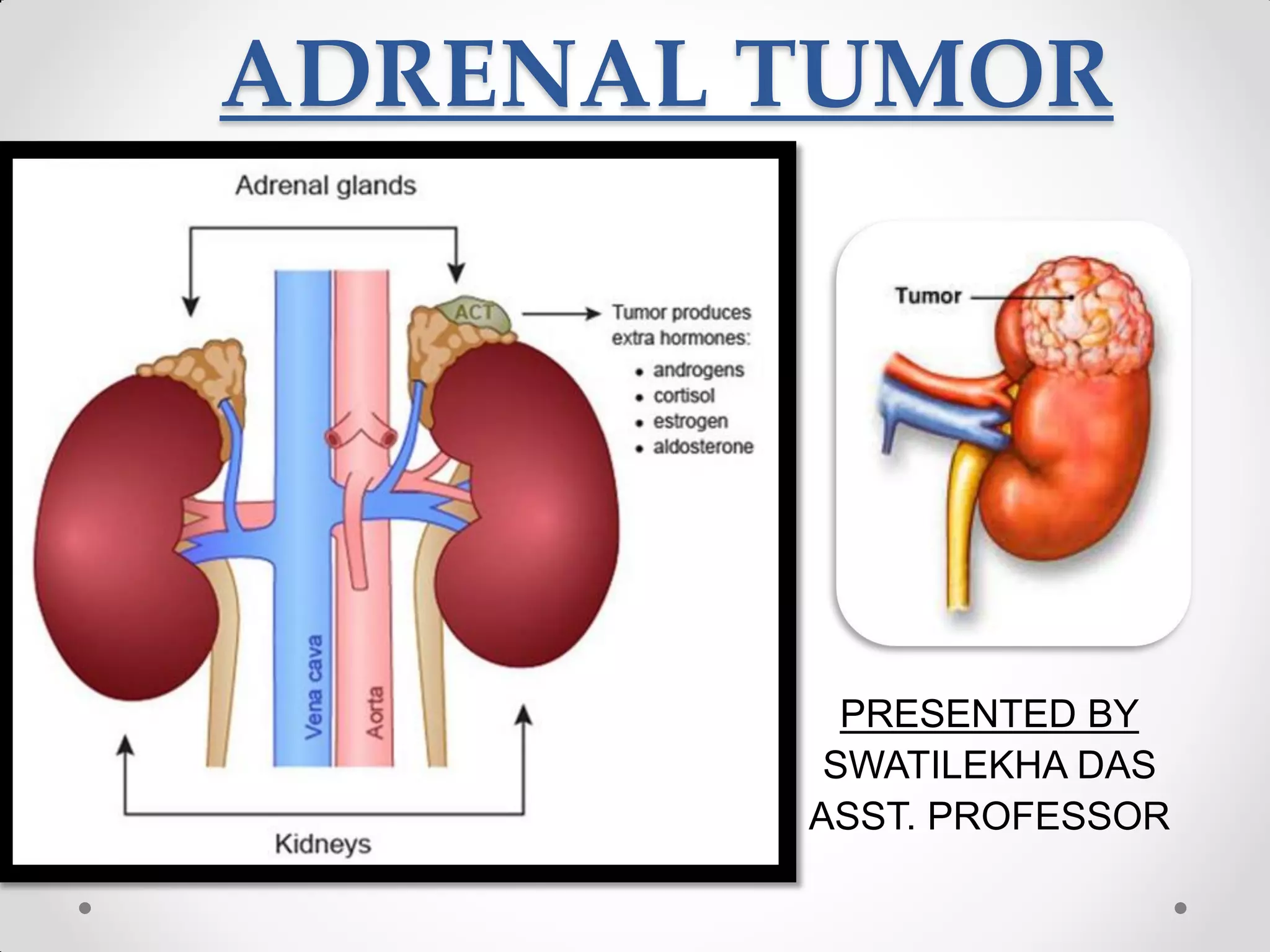
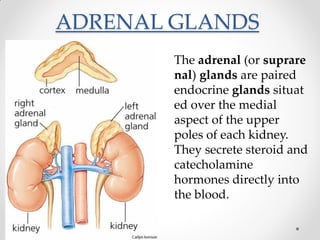
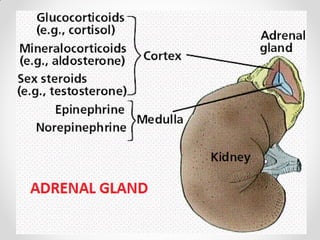
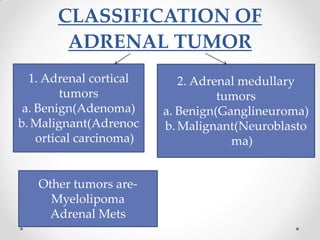
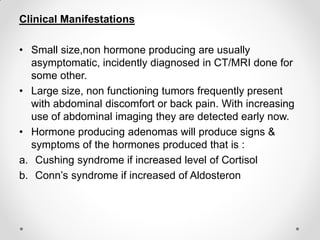
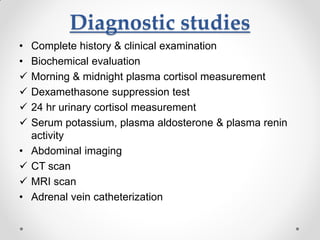
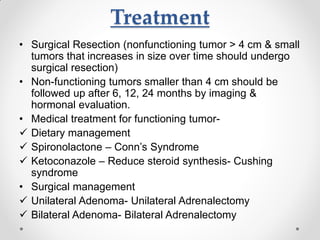
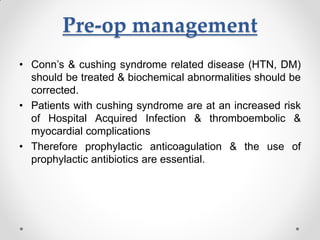
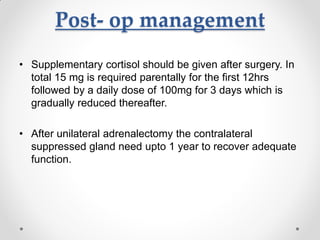
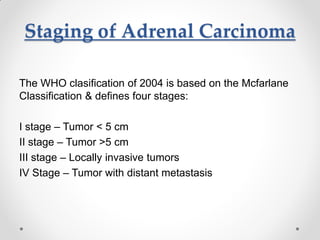
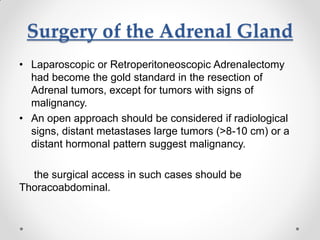
The document provides an overview of adrenal tumors, including their classification into adrenal cortical and medullary tumors, and discusses benign and malignant forms. It details the clinical manifestations, diagnostic studies, and treatment options including surgical resection and medical management for hormone-producing tumors. The document also addresses the management of adrenal malignancies such as adrenocortical carcinoma, including diagnostic approaches and the importance of follow-up care post-surgery.