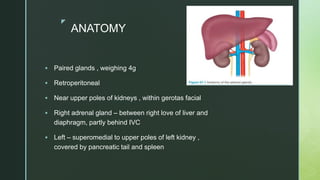
The document details adrenal tumors' anatomy, physiology, and management, highlighting various types including incidentalomas, adrenocortical carcinoma, pheochromocytoma, and neuroblastoma. It discusses diagnosis methods such as imaging, laboratory tests, and treatment approaches including surgery and medication. Additionally, it outlines the characteristics and clinical features associated with these tumors, emphasizing the importance of proper assessment and intervention.