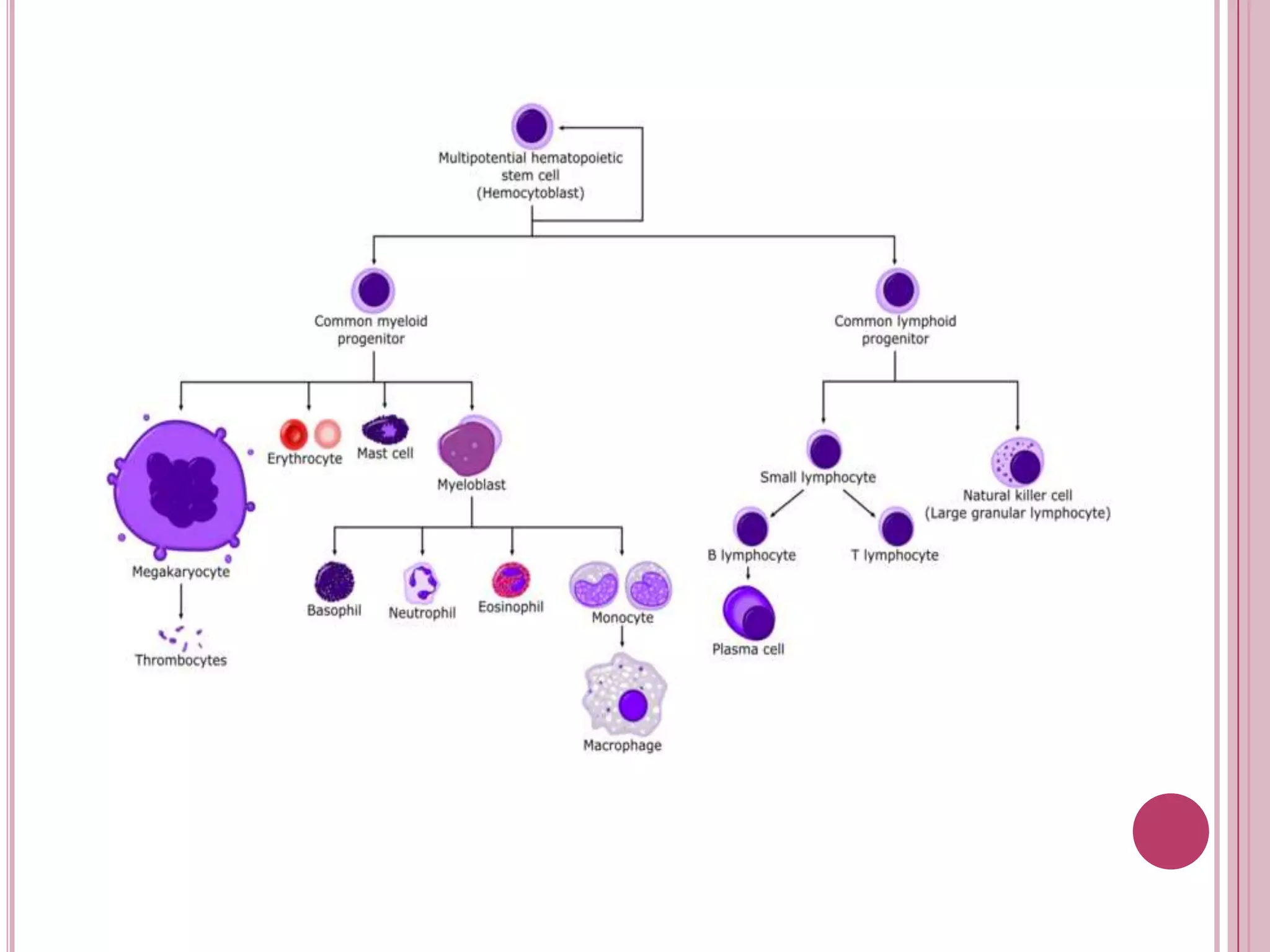
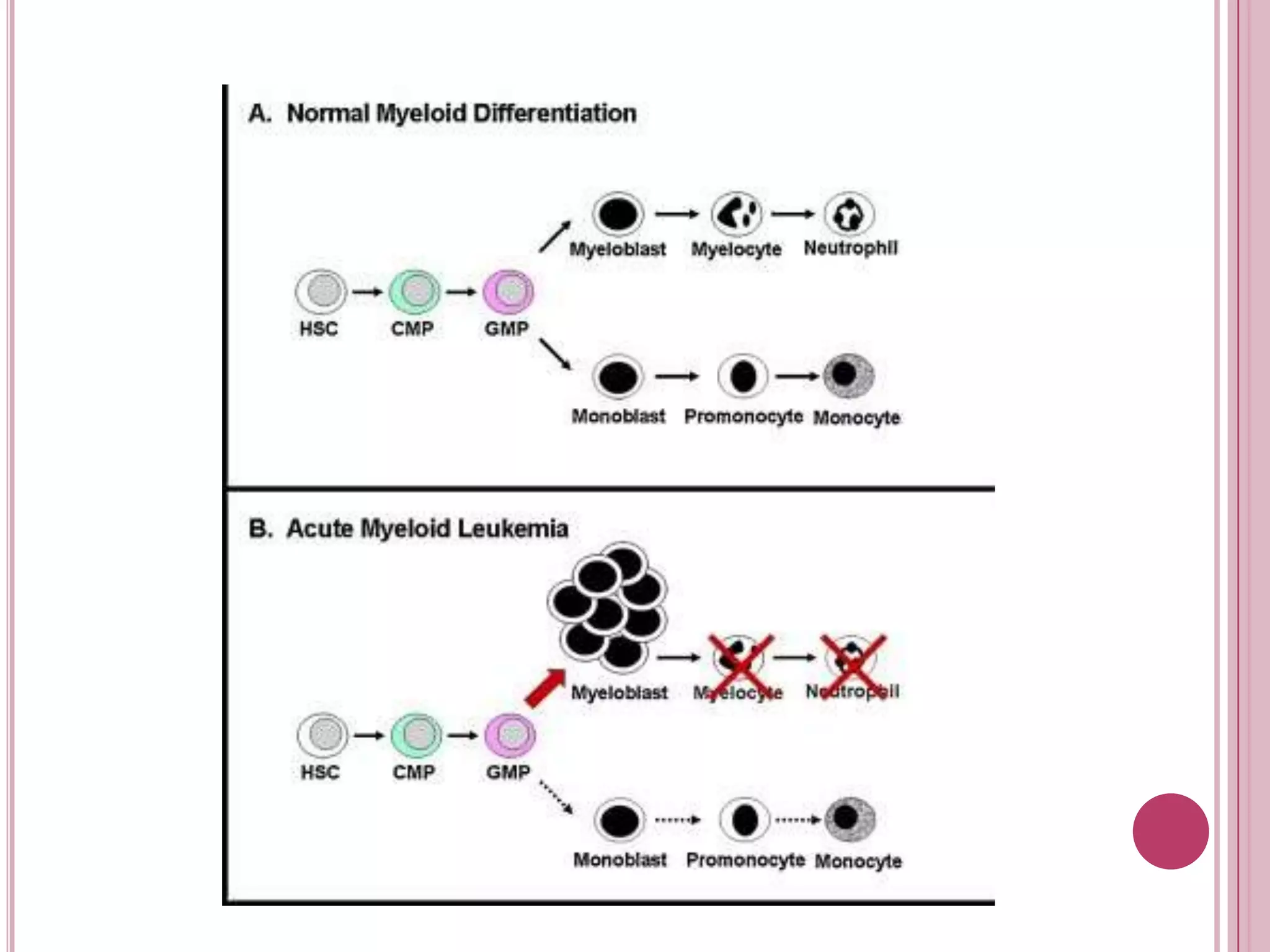
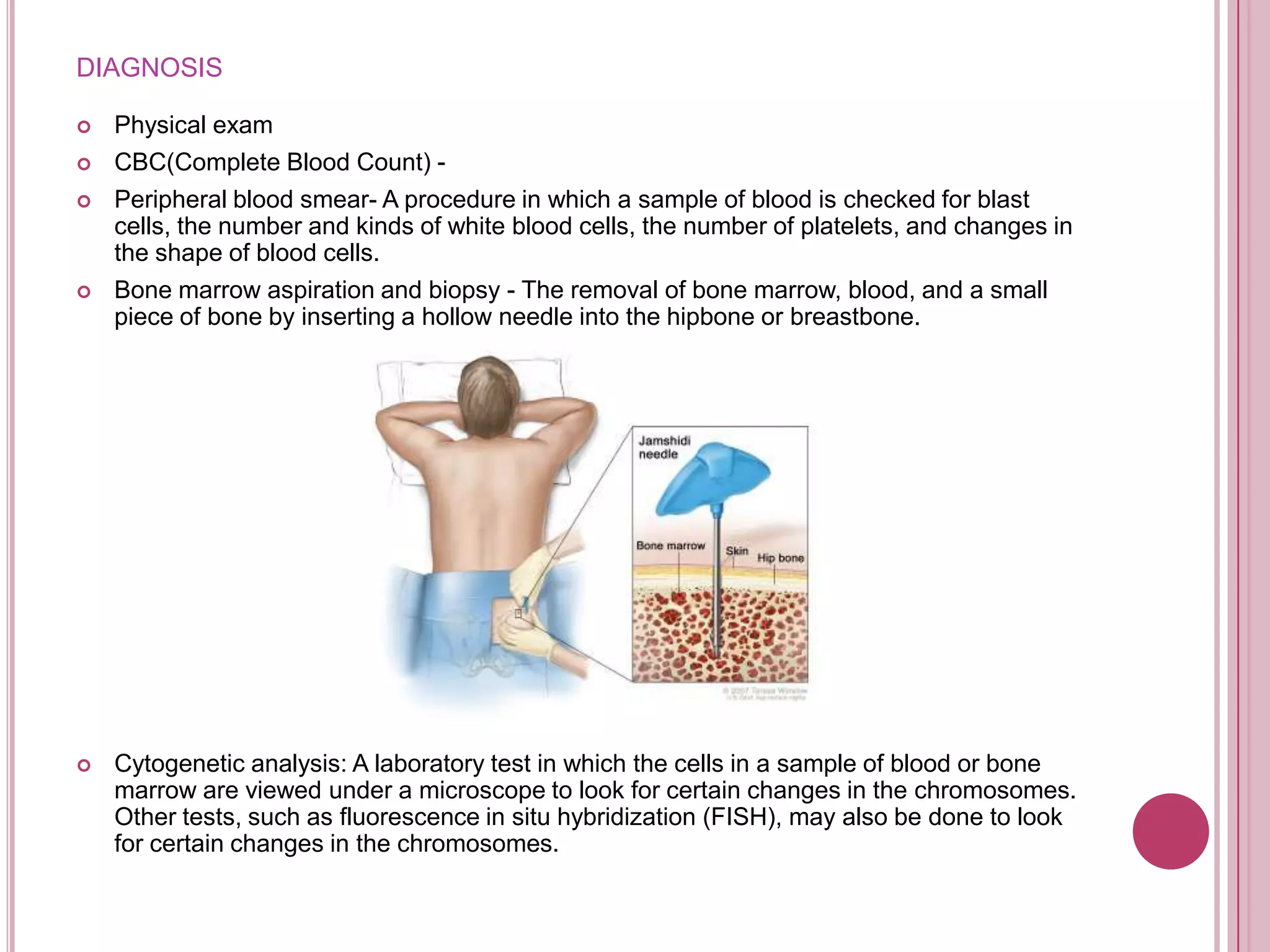
Acute myelogenous leukemia (AML) is a cancer of the blood and bone marrow characterized by the rapid growth of abnormal white blood cells that build up in the bone marrow and interfere with normal blood cell production. AML results from genetic mutations that cause immature myeloid cells to proliferate uncontrollably. Diagnosis involves blood tests, bone marrow aspiration and biopsy, and cytogenetic analysis. Treatment consists of induction chemotherapy to achieve remission followed by consolidation chemotherapy to destroy any remaining leukemia.