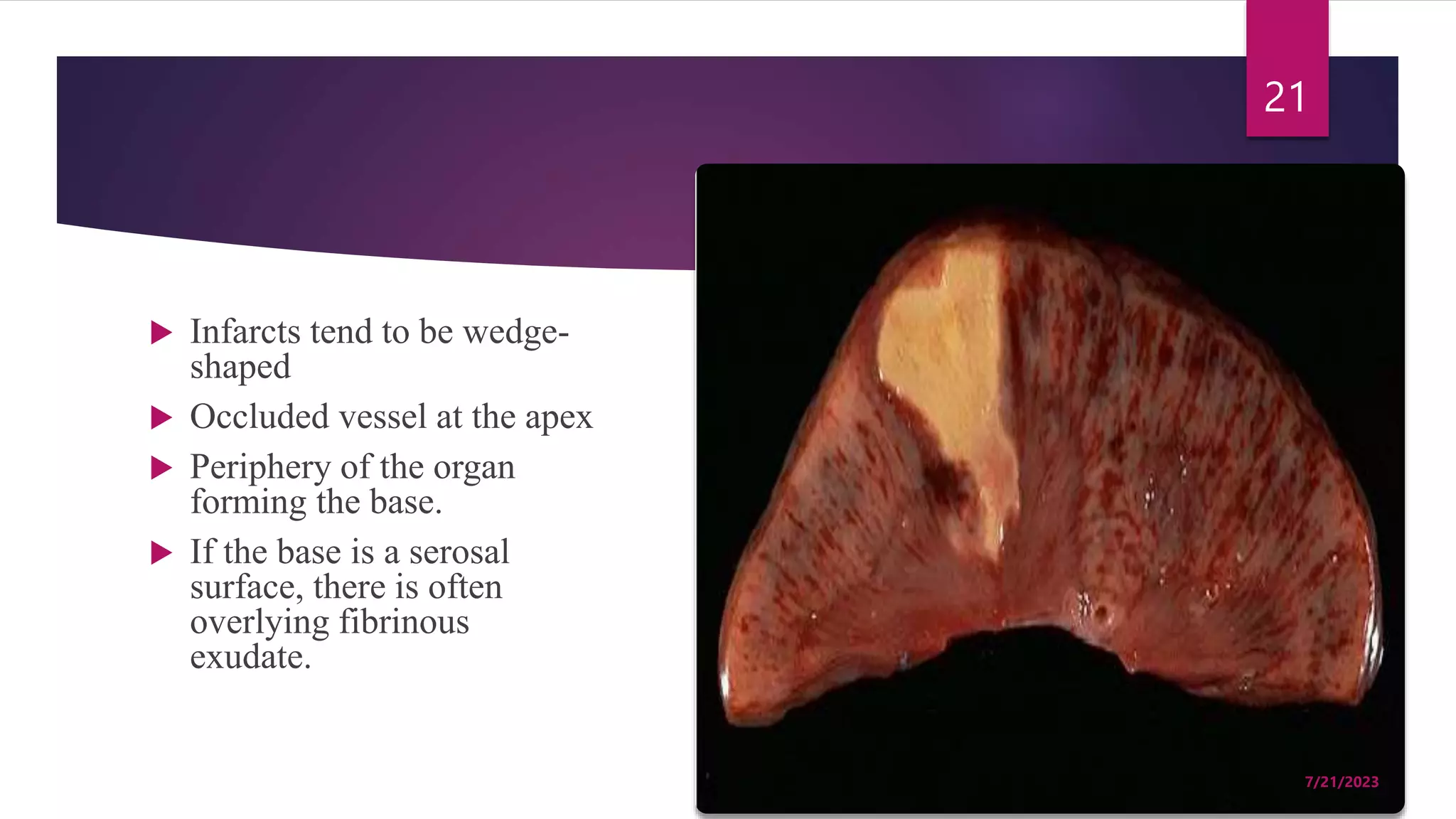
The document discusses various types of embolism, infarction, and shock, including definitions, causes, symptoms, and management. It details thromboembolic causes such as those from deep venous thrombosis, fat emboli associated with fractures, gas emboli from decompression sickness, and amniotic fluid emboli during labor. Additionally, the document describes shock types, their clinical presentations, stages, and management strategies, highlighting specific conditions like hypovolemic, cardiogenic, obstructive, and distributive shock.