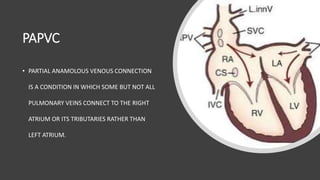
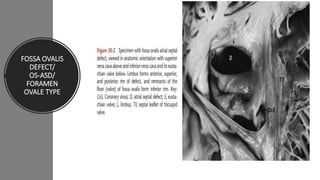
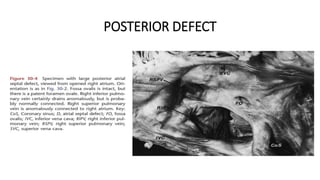
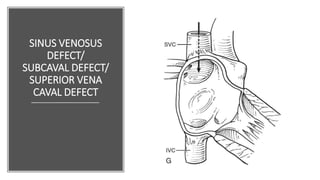
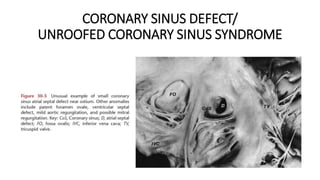
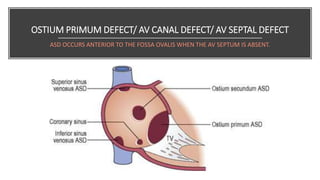
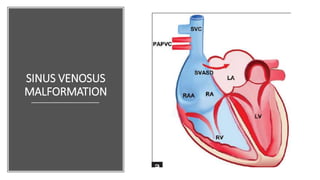
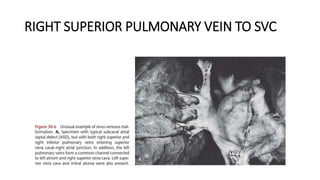
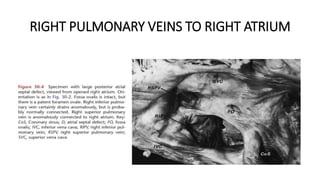
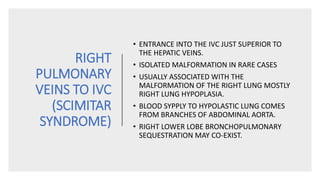
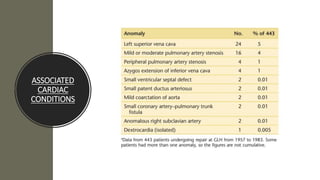
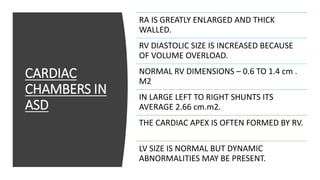
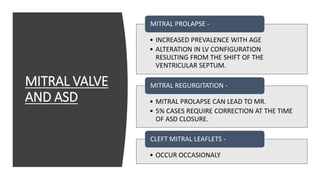
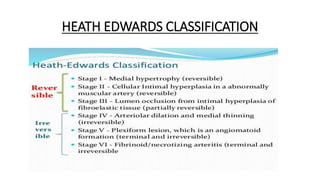
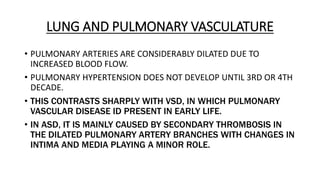
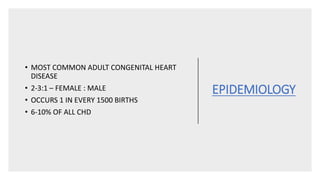
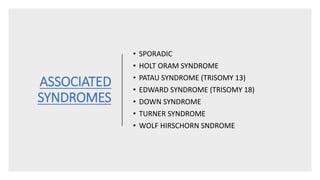
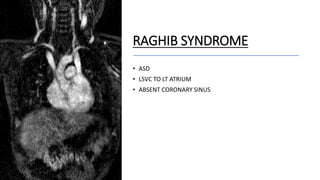
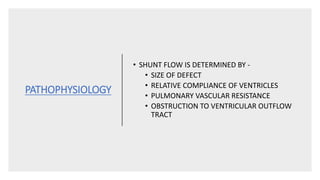
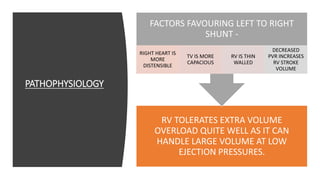
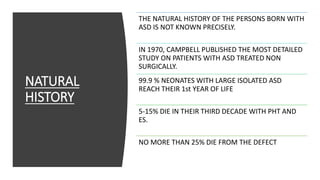
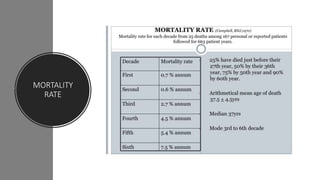
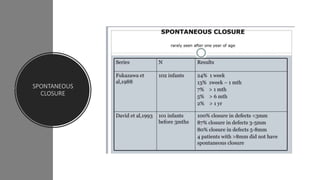
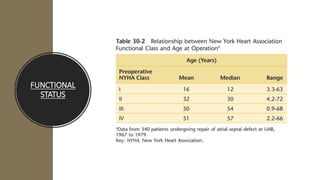
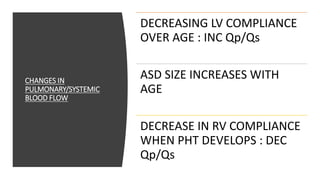
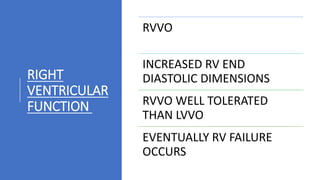
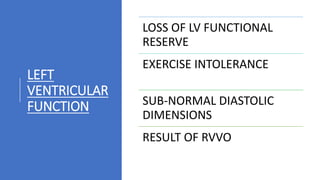
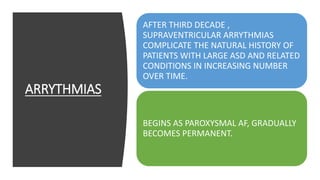
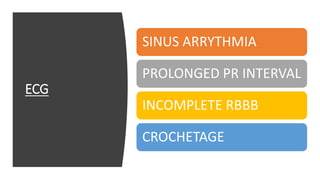
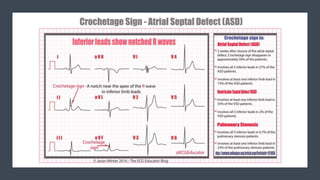
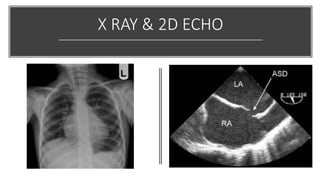
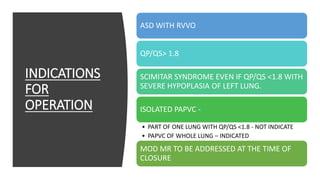
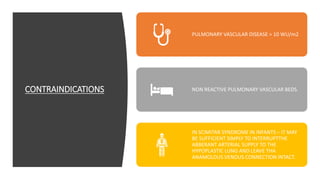
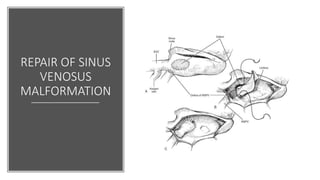
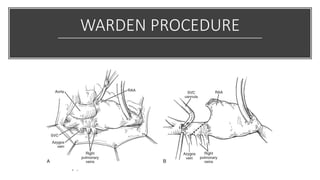
This document provides an overview of atrial septal defects (ASD), including definitions, types, development, associated conditions, clinical presentation, investigations, and treatment. The main types of ASD are fossa ovalis/ostium secundum, sinus venosus, and ostium primum defects. Clinical features may include fatigue, breathlessness, and arrhythmias. Investigations include chest X-ray, echocardiogram, and cardiac catheterization. Large defects or those causing heart failure or pulmonary hypertension typically warrant surgical closure to repair the septal defect. The surgery aims to close the defect without causing heart block or valve problems.