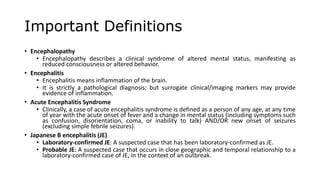
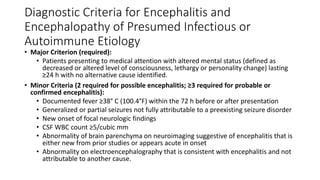
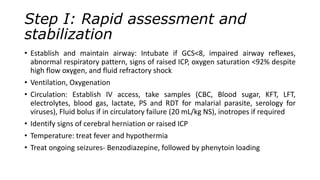
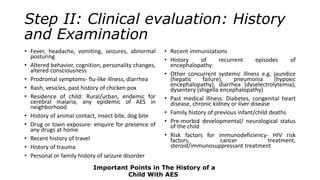
This document provides information about acute encephalitis syndrome, including important definitions, diagnostic criteria, and guidelines for evaluation and management of children presenting with acute encephalitis. It defines acute encephalitis syndrome as a person of any age with acute fever and altered mental status including confusion, disorientation or seizures. It outlines a six step approach to rapidly assess and stabilize the patient, conduct a clinical evaluation, perform investigations, provide empirical treatment, supportive care and treatment, and prevent complications through rehabilitation.