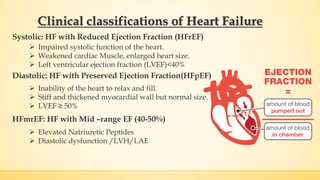
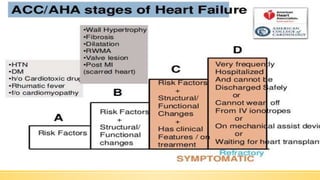
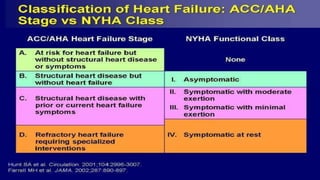
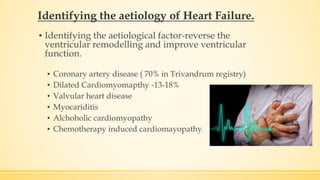
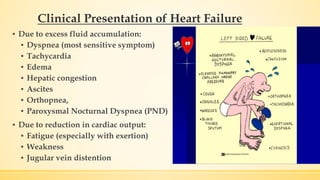
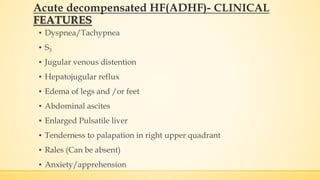
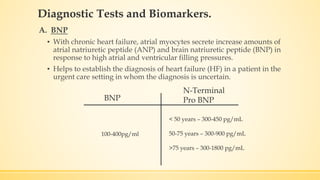
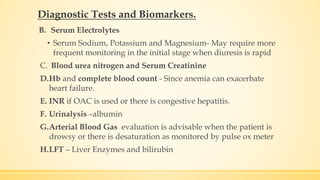
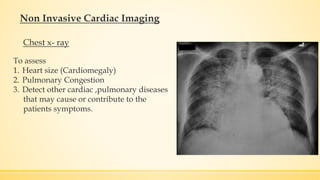
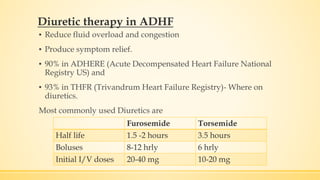
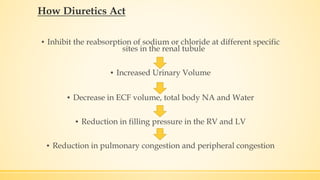
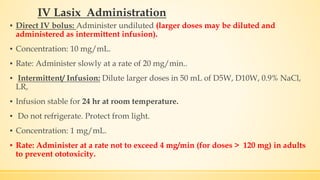
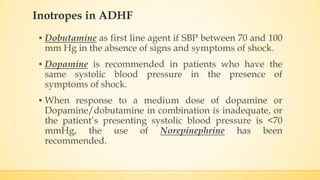
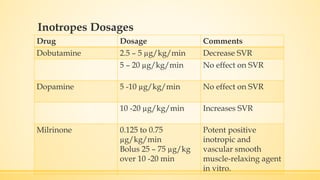
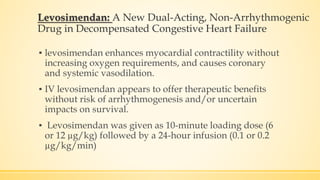
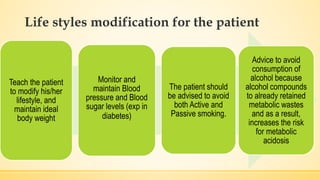
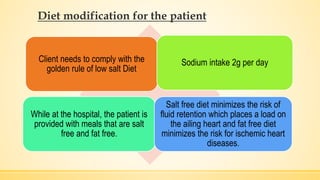
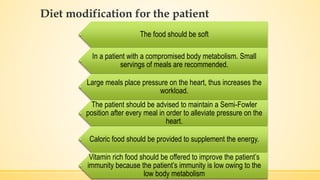
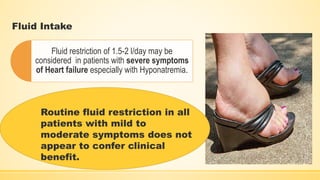
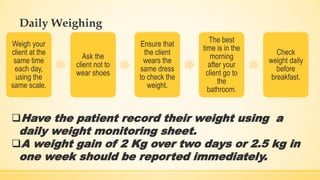
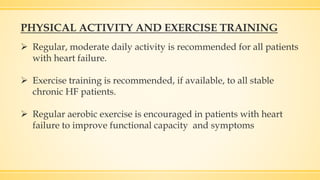
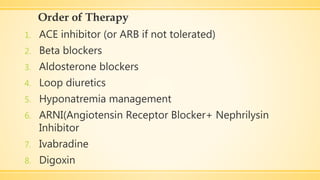
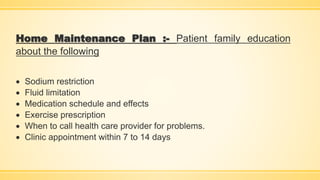
The document provides information on competencies for nurses caring for patients with heart failure. It defines heart failure and describes the different clinical classifications. It discusses identifying the underlying causes, nursing management including monitoring clinical parameters, diagnostic tests and biomarkers, medical management with diuretics and inotropes, and lifestyle modifications including diet and risk factor reduction for chronic heart failure patients.