This document discusses acetabular fractures and hip dislocations. It covers the epidemiology, anatomy, mechanisms of injury, clinical evaluation, radiographic evaluation, classification, treatment, complications, and hip dislocations. Some key points are:
- Acetabular fractures occur in 3 per 100,000 people per year and can cause neurologic injuries in up to 30% of cases, usually involving the sciatic nerve.
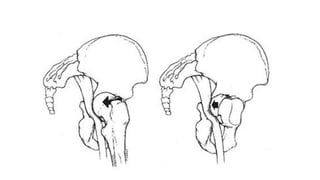
- The acetabulum has anterior and posterior columns that form an inverted Y shape and support the hip joint.
- Injuries are usually from high-energy trauma and the fracture pattern depends on the position of the hip at injury.
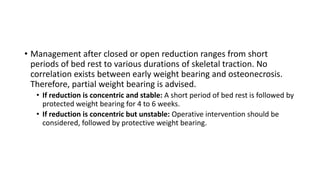
- Treatment goals are anatomic restoration