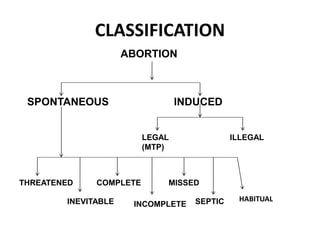
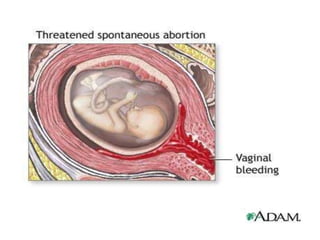
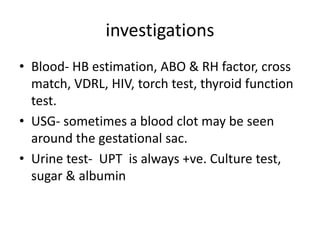
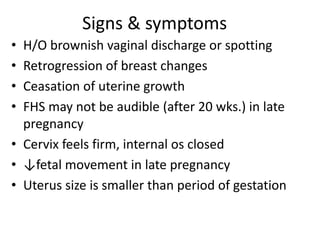
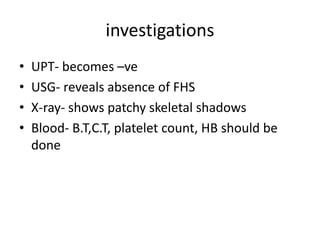
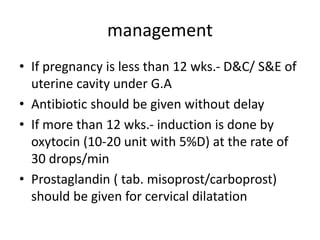
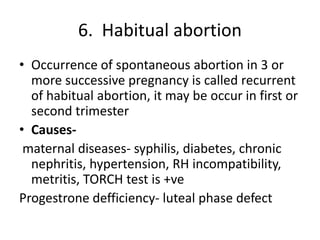
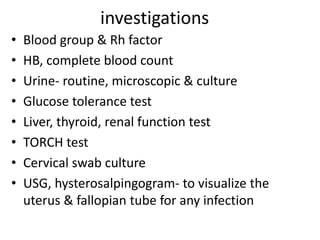
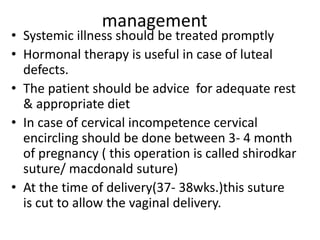
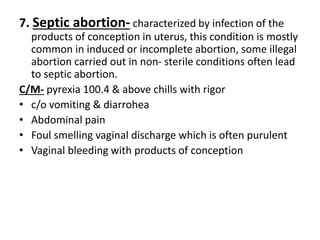
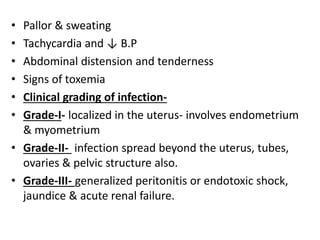
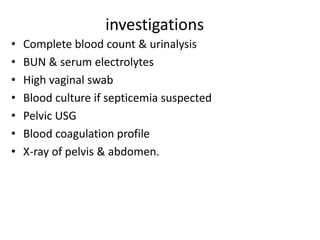
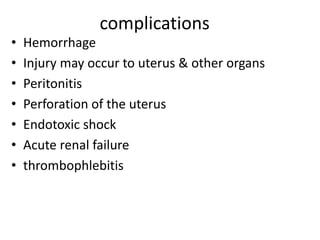
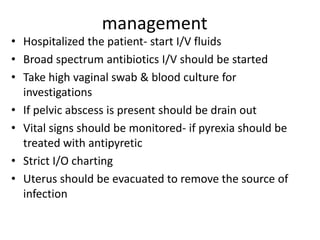
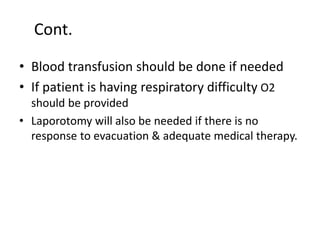
This document discusses various types of abortion, including spontaneous, threatened, inevitable, complete, incomplete, missed, septic, and habitual abortion. It defines abortion as the expulsion of the fetus weighing less than 1000g before 28 weeks gestation. Spontaneous abortion is the involuntary loss of pregnancy before 28 weeks. Causes can be maternal, fetal, or immunological factors. Treatment depends on the type but may include bed rest, medication, or surgical evacuation of the uterus. The document also covers medical termination of pregnancy (legal abortion) and various methods used in the first and second trimesters.