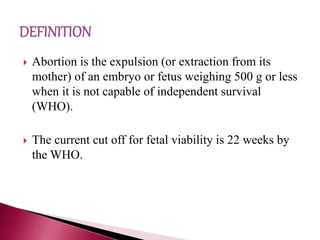
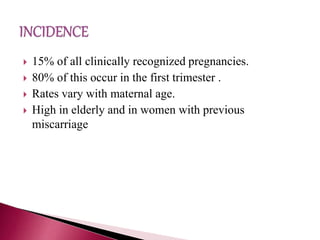
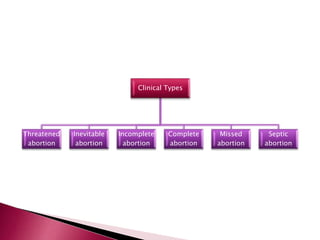
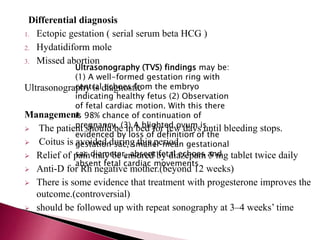
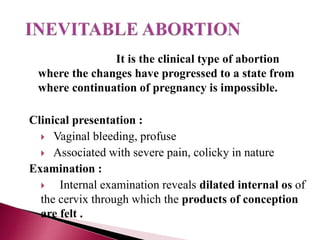
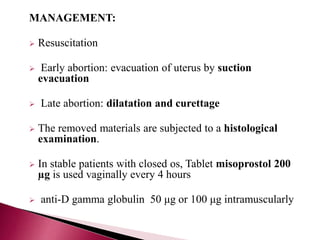
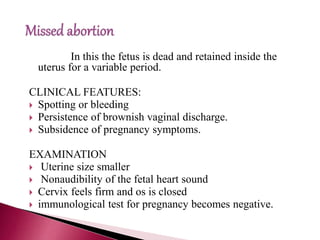
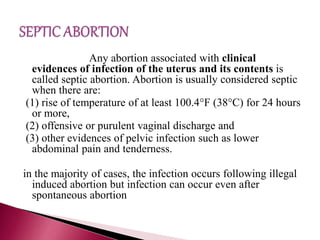
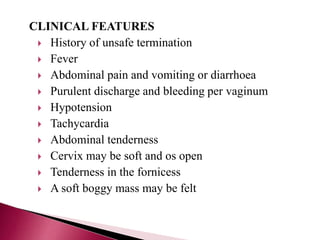
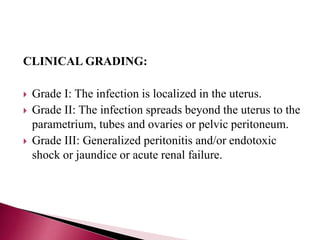
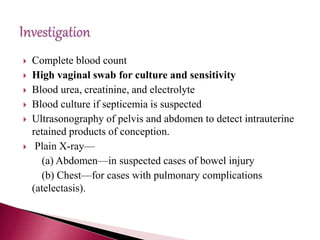
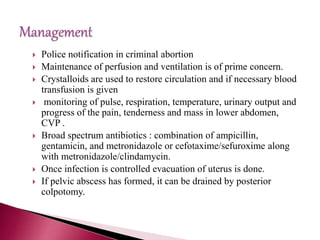
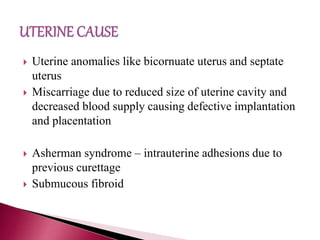
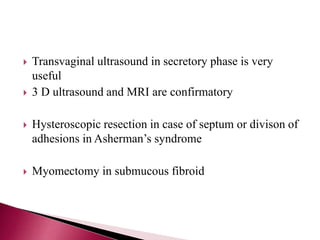
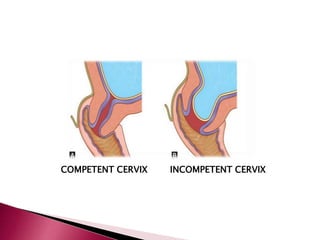
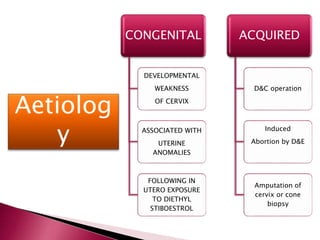
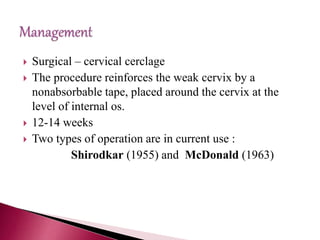
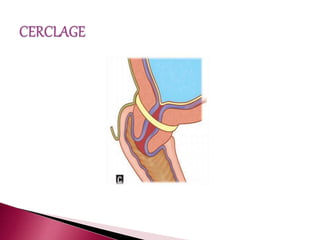
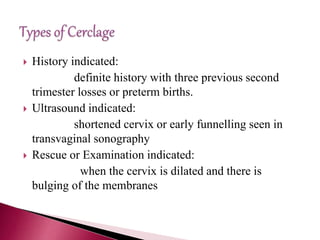
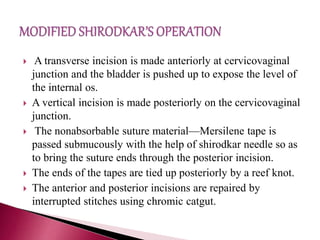
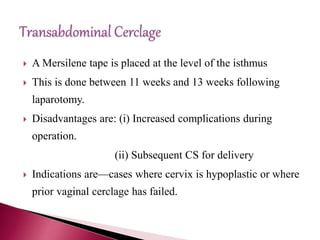
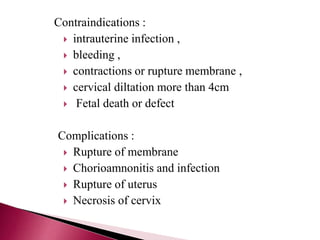
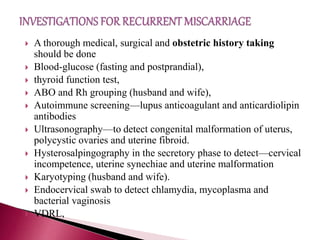
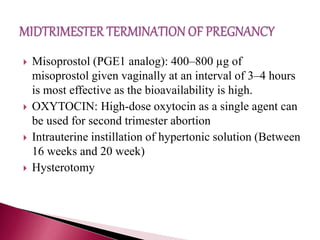
The document provides a comprehensive overview of abortion types, causes, and management, detailing clinical presentations such as vaginal bleeding, cramping, and uterine examination findings. It addresses specific conditions like missed abortion, incomplete miscarriage, and septic abortion, outlining the diagnostic tools and treatment options available, including medical and surgical interventions. Additionally, it discusses recurrent miscarriage and cervical insufficiency, highlighting risk factors, diagnostic approaches, and management techniques including cervical cerclage.