1) The document discusses gravidity, parity, and the signs and symptoms of bleeding in early pregnancy. Gravidity refers to the number of pregnancies and parity refers to the number of viable pregnancies.
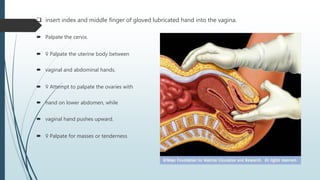
2) Examination of a pregnant woman with vaginal bleeding involves general examination, abdominal examination, pelvic examination, speculum examination, and bimanual examination to check for signs of bleeding, masses, cervical changes, and tenderness.
3) Common causes of bleeding in early pregnancy include miscarriage, ectopic pregnancy, molar pregnancy, and other potential issues like placental problems or abnormalities. Management options for miscarriage include surgical, medical, and natural approaches.


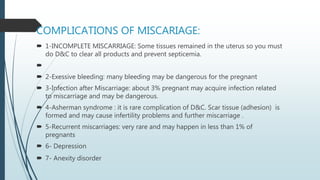

![1-Call your physician or go to the emergency room if tissue,
fluid, or what appears to be clumps of blood come out of your
vagina
If you do pass tissue that you think might be fetal tissue, put it in a
clean, sealed container and take it with you to the doctor.
2-Recognize that you may be at risk of miscarrying if you have
spotting or vaginal bleeding
3-Take note if you experience lower back pain
4-Recognize the symptoms of a septic miscarriage.
Symptoms include:[7][8]
•Fluid coming from your vagina that smells bad.
•Vaginal bleeding.
•Fever and chills.
•Cramping and pain in your abdomen](https://image.slidesharecdn.com/pbl3-170515163510/85/bleeding-in-early-pregnancy-38-320.jpg)