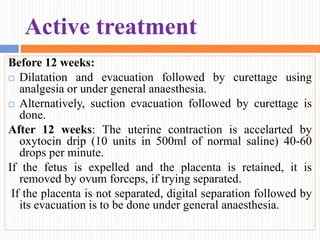
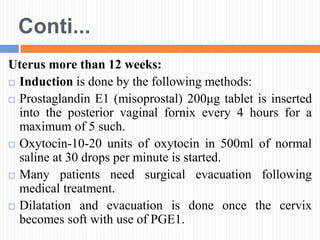
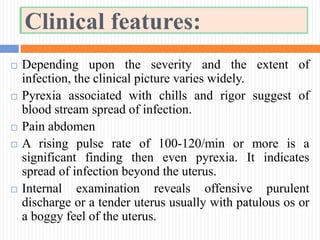
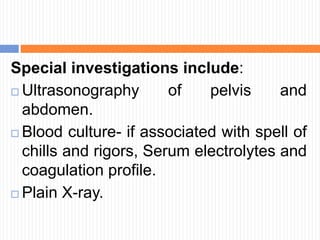
The document defines abortion and discusses its classification, incidence, etiology, and management. It notes that abortion is the expulsion of an embryo or fetus weighing 500 grams or less before 22 weeks of gestation. Abortions are classified as spontaneous, threatened, inevitable, complete, incomplete, missed, or septic. The incidence of abortion in India is estimated at 10-20% of pregnancies. Complications of abortion include hemorrhage, infection, and future obstetric or gynecological issues. The role of nurses is to assess for complications, provide support and education, and monitor for issues like shock.