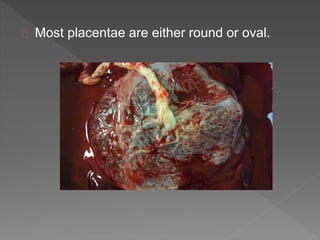
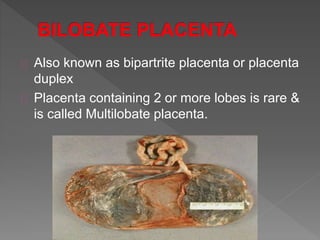
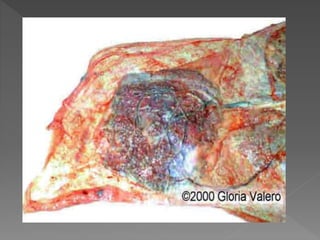
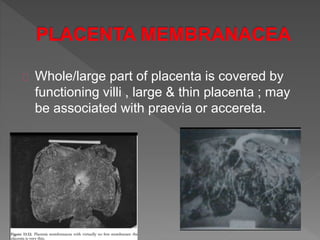
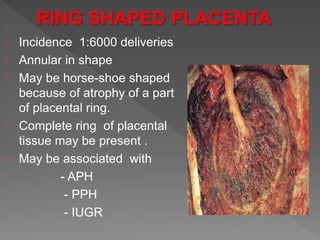
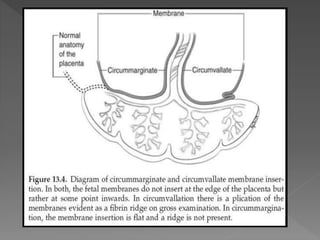
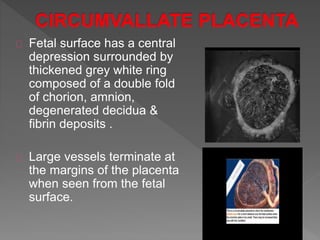
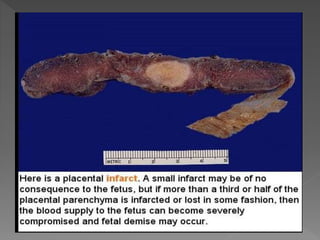
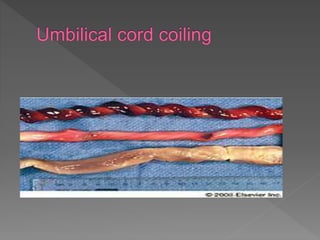
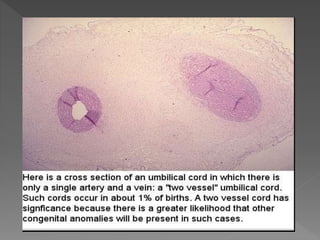
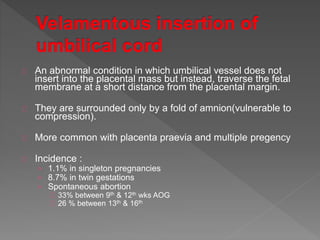
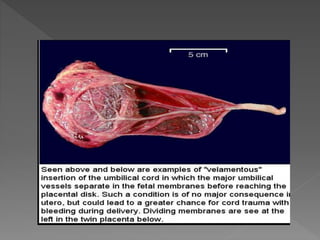
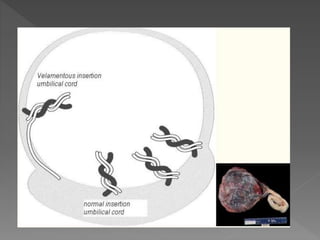
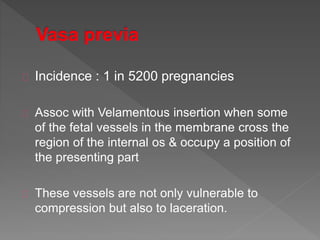
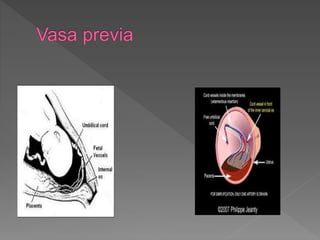
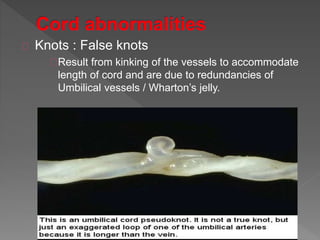
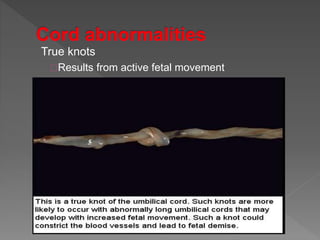
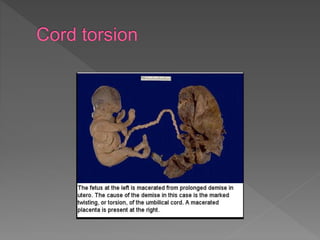
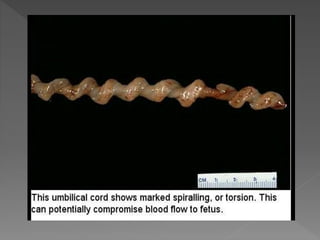
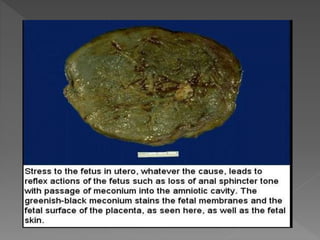
The document summarizes various placental and umbilical cord abnormalities. It describes the typical shapes of most placentae as round or oval but notes that variations are common, including multiple placentae or bilobed placentae. It also discusses abnormalities in placental structure, cord insertion sites, umbilical cord vessels, and other variations that can occur in the placenta and umbilical cord. Many of these abnormalities are associated with risks like abnormal fetal growth, preterm delivery, fetal distress, or hemorrhage. The document provides details on the incidence, risk factors, pathogenesis, and clinical implications of numerous placental and umbilical cord variations.