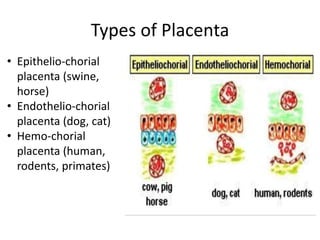
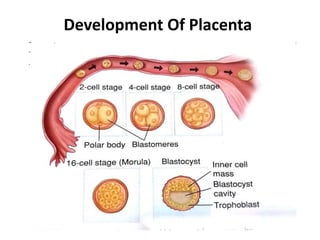
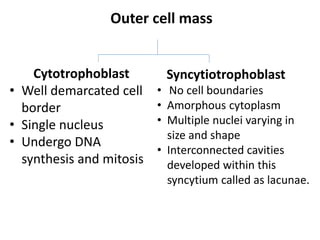
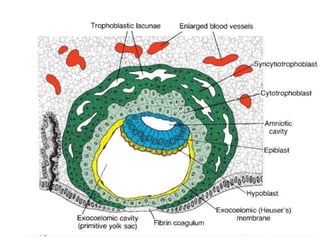
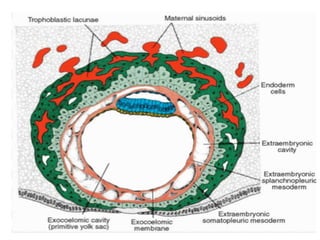
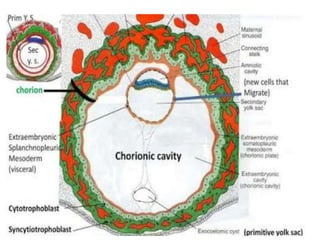
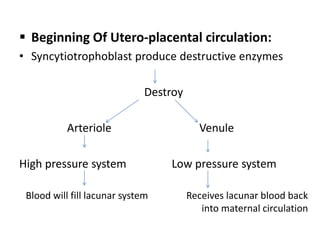
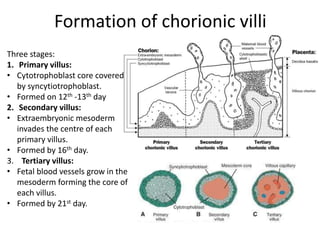
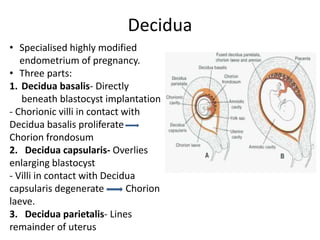
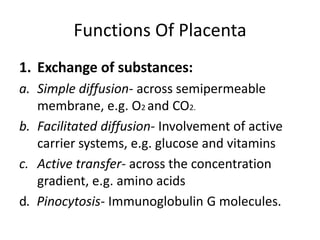
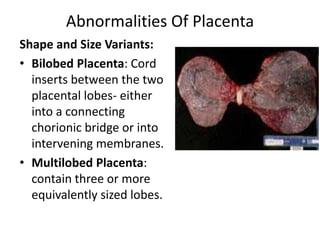
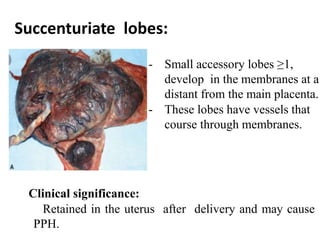
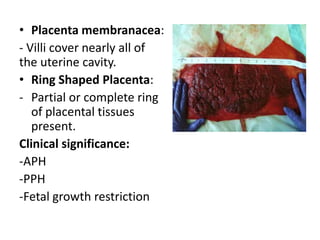
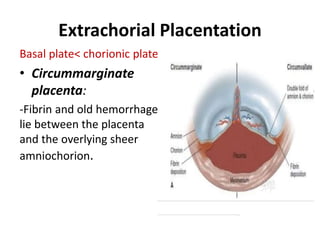
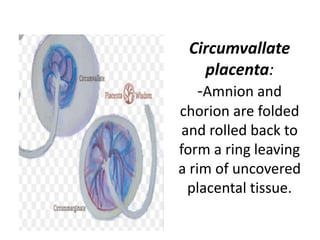
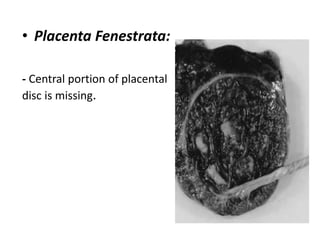
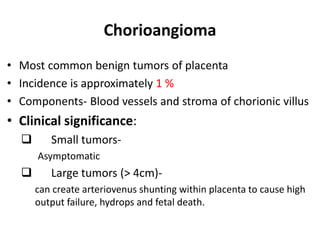
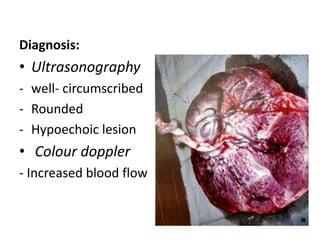
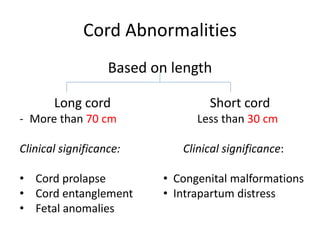
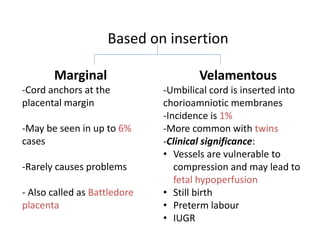
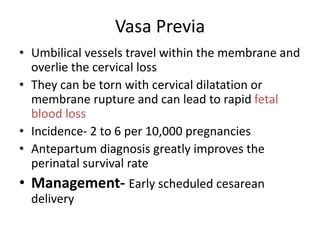
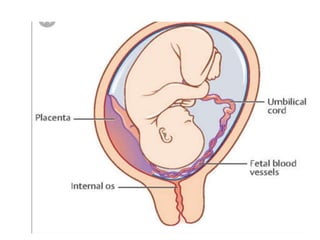
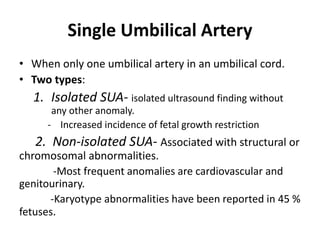
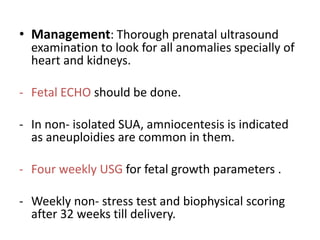
The document describes the anatomy and development of the placenta and discusses some common abnormalities. It notes that the placenta establishes a connection between the mother and fetus to allow for nutrient/waste exchange. During development, trophoblast cells form villi that invade the uterine wall. The three layers of the placenta each have specific functions in nutrient exchange and hormone production. Some abnormalities can cause issues like abnormal bleeding, fetal growth restriction, or stillbirth if not properly managed. Ultrasound is used to diagnose many placental abnormalities prenatally.