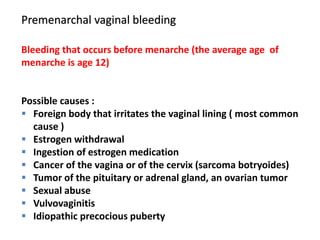
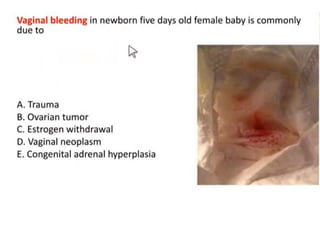
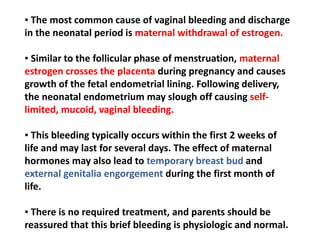
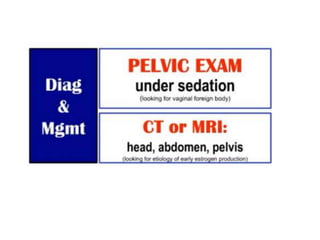
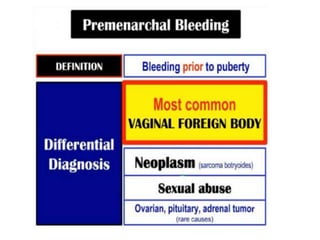
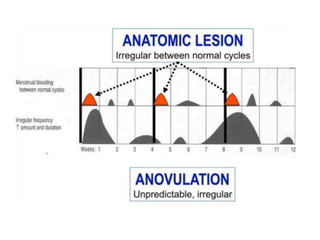
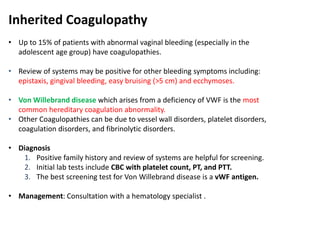
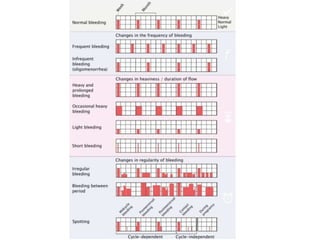
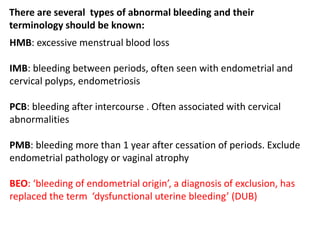
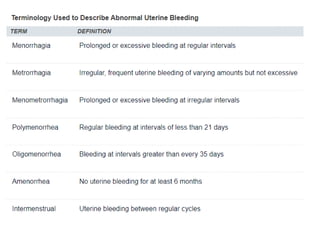
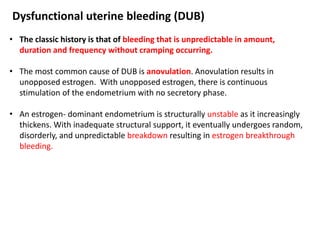
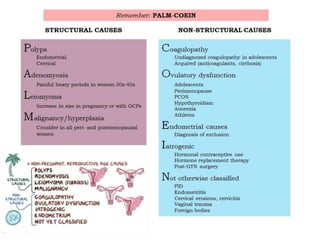
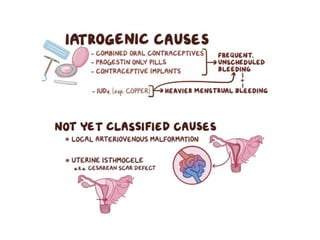
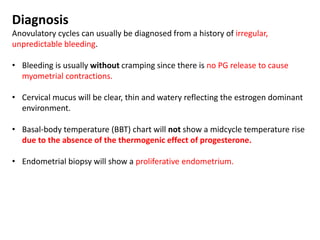
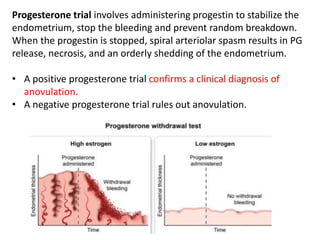
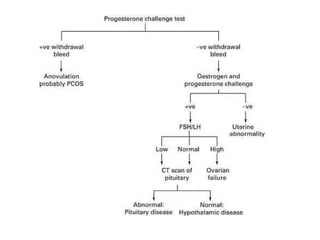
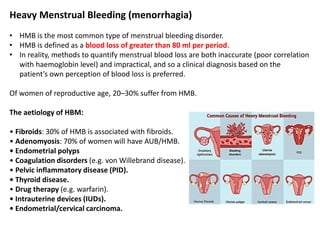
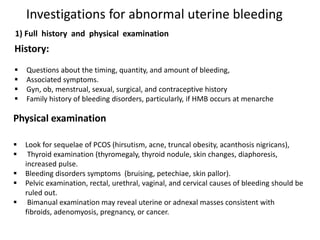
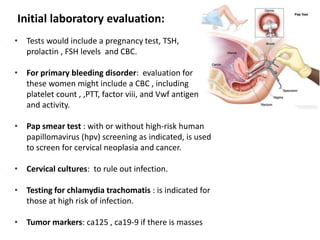
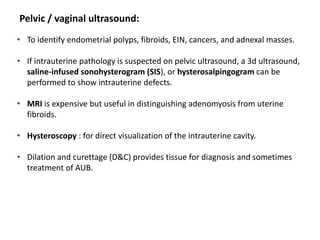
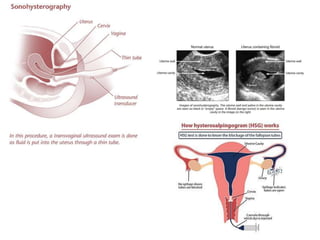
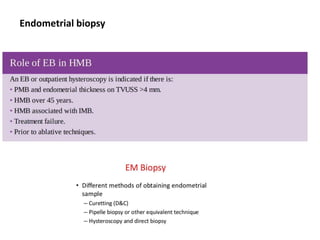
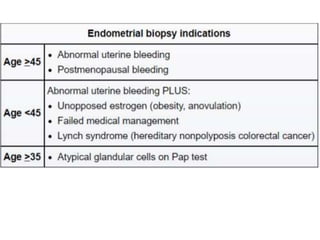
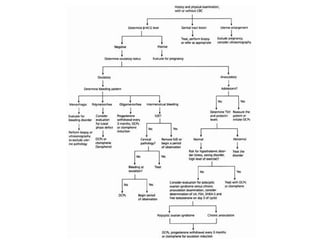
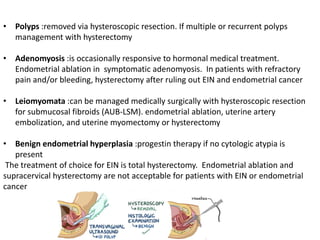
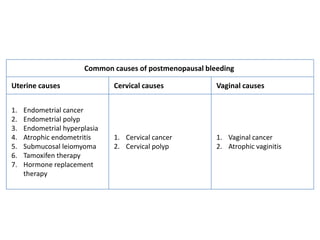
This document discusses abnormal vaginal bleeding, classifying it as premenarchal, reproductive age, or postmenopausal bleeding. It describes various causes for each type of bleeding such as foreign bodies, cancers, hormonal imbalances. Evaluation involves history, exam, pregnancy tests, ultrasounds, and potentially endometrial biopsies. Common causes of abnormal reproductive age bleeding include pregnancy, anatomical issues, inherited bleeding disorders, and dysfunctional uterine bleeding from anovulation.