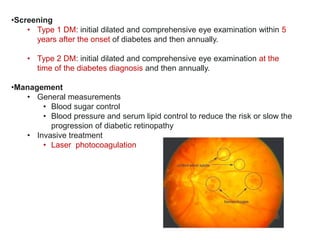
Chronic complications of diabetes mellitus include macrovascular complications like atherosclerosis and coronary artery disease, as well as microvascular complications involving the eyes, kidneys, and nerves. Key microvascular complications include diabetic nephropathy, the leading cause of end-stage renal disease; retinopathy, the most common cause of blindness; and neuropathy resulting in numbness, pain, and increased risk of foot ulcers and infection. Management involves controlling risk factors like hypertension and hyperglycemia, as well as treatments tailored to each complication such as ACE inhibitors for nephropathy and laser therapy for retinopathy.