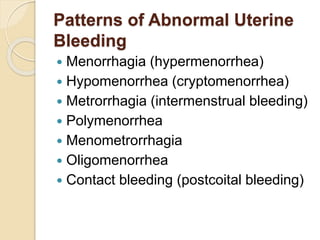
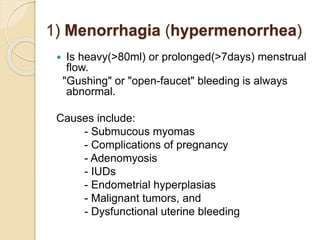
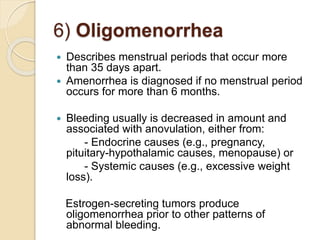
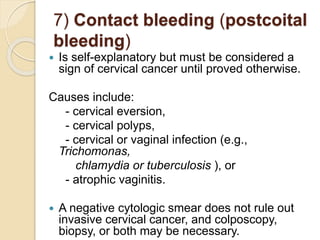
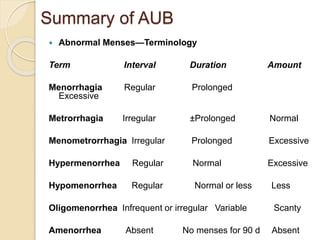
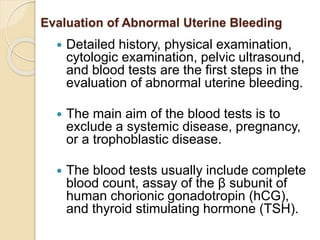
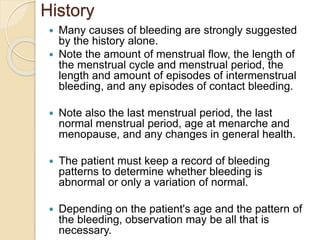
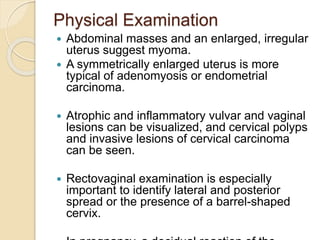
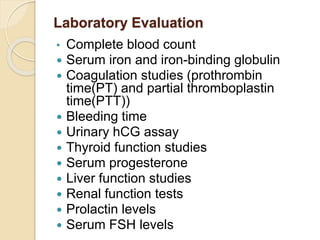
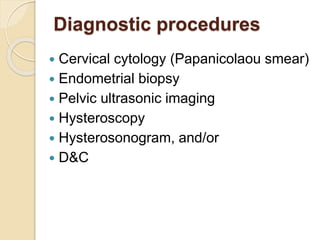
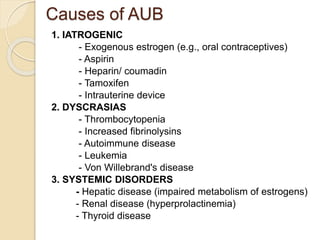
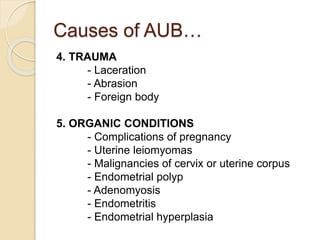
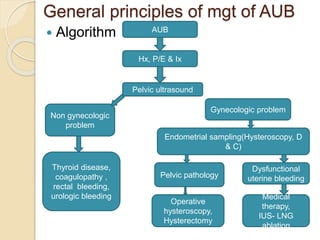
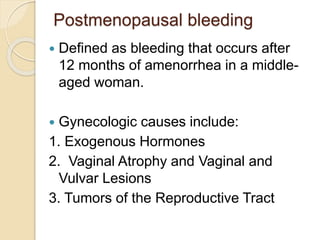
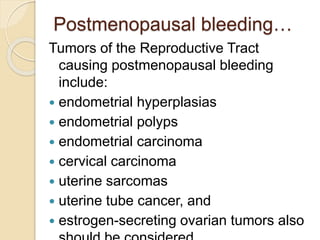
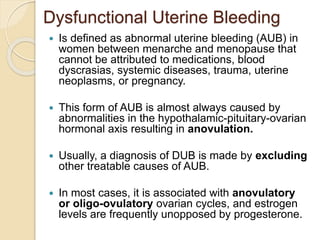
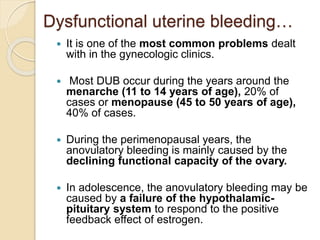
Abnormal uterine bleeding includes heavy, prolonged, irregular or abnormal menstrual bleeding that can be caused by various gynecological or systemic conditions. A thorough history, physical exam, blood tests and diagnostic imaging are used to evaluate the bleeding and identify potential causes. Dysfunctional uterine bleeding, one of the most common causes, is attributed to anovulation and unopposed estrogen levels resulting in irregular bleeding. Treatment involves hormonal regimens or surgical procedures if hormones do not control the bleeding.