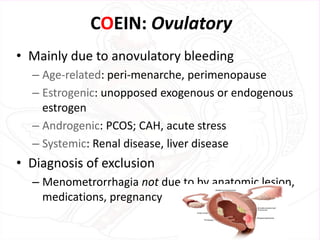
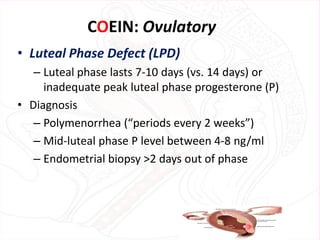
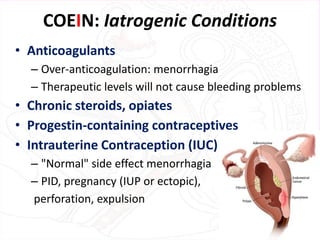
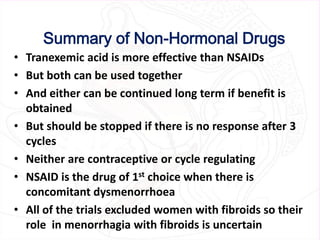
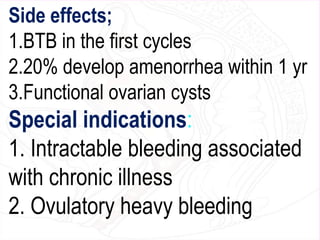
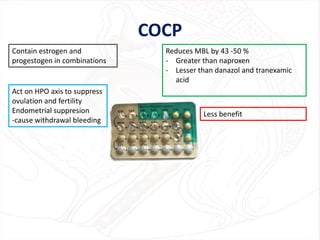
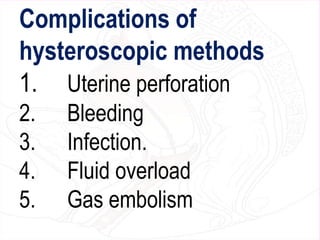
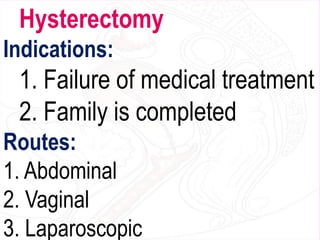
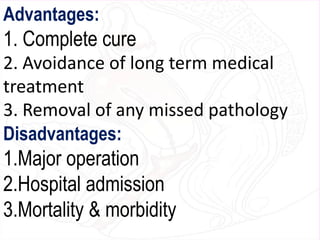
This document provides information on the evaluation and management of abnormal uterine bleeding (AUB). It begins with definitions of terms and classifications of AUB. Evaluation involves a history, physical exam, and testing as needed which may include ultrasound, hysteroscopy, or endometrial biopsy to determine the cause. Causes are categorized using the FIGO PALM-COEIN system. Treatment options discussed include general measures, medical therapies like hormones, NSAIDs, tranexamic acid, and surgical procedures such as endometrial ablation or hysterectomy. Non-hormonal and hormonal medical treatments are summarized. The document concludes with a discussion of progestin therapies.