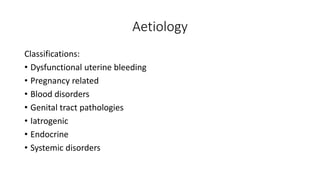
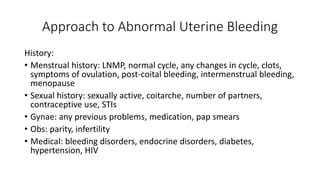
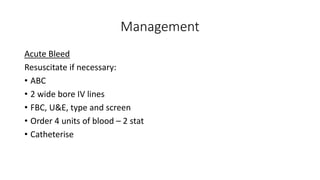
Abnormal uterine bleeding can have various causes and presentations. It includes heavier or longer than normal periods, bleeding between periods or after menopause. Evaluation involves history, examination, and tests to identify potential issues like fibroids, pregnancy complications, or endocrine disorders. Treatment depends on the underlying cause but may involve hormonal therapy, surgical procedures like endometrial ablation, or hysterectomy in some cases.